Kavya Chaganti: I’ve seen a drop in patients coming in for STI checks
GP Dr Kavya Chaganti says she’s noticed less people coming in for a very important check up in recent years due to this incorrect assumption.

Sexual Health
Don't miss out on the headlines from Sexual Health. Followed categories will be added to My News.
The rates of sexually transmitted infections (STIs) have been rising, (particularly since the pandemic).
Testing rates are not as high as we’d like, and treatment guidelines have been evolving thanks to antibiotic resistance.
In my own clinic in recent years, I’ve noticed fewer patients are coming in specifically requesting STI checks.
Most of the STI checks I do now are offered opportunistically, when my patients present with a different issue.
When it comes to STIs, many people incorrectly assume they will have noticeable signs or symptoms alerting them that something is wrong.
The reality is STIs are often invisible.

Chlamydia, for example, shows no symptoms in up to 90 per cent of people.
STIs are also very common: according to health.gov.au, around one in six people report having an STI in their lifetime.
STI testing is simple and usually involves a urine test and blood test, and sometimes a swab. Understandably, people might feel awkward about asking for one.
However I think patients should be proud of being smart and responsible about their sexual health. Sex is a normal part of life, STIs are common, and regular checks are important as many infections are asymptomatic.
Healthcare professionals are trained to provide a confidential and non-judgmental space for these conversations.
A good doctor will listen, ask about your sexual health history, examine you if needed, and guide you on how often to test based on your lifestyle and risk factors.
In general, I would recommend you have an STI check when:
• You’re starting or ending a relationship
• After unprotected sex
• If your partner has an STI
• If you have multiple partners or frequent change in partners
• Methamphetamine use is also a risk factor for STIs
You should also see your doctor anytime you notice symptoms, even if you’ve had a recent check.
Any rashes, lumps, bumps, soreness, discharge, pain during intercourse or when you pass urine should be checked.
If you suspect you might have an STI, it’s best to avoid sex (even with condoms) until you’ve seen a doctor.
Some infections, like hepatitis or HIV, can take time to show up on a test so your doctor may recommend getting testing now and again in a few weeks, or at regular intervals depending on your exposure and risk factors.
If you test positive for an STI, your doctor will talk to you about whether you need to abstain from sex, and for how long. Many STIs can be easily treated. Some do require ongoing monitoring and management. Even HIV (though not curable) can now be effectively managed with antiretroviral medication to reduce the risk of progression to AIDS. Regular checks allow prompt treatment, which helps reduce the risk of complications like pelvic inflammatory disease, fertility difficulties, and other chronic health issues.

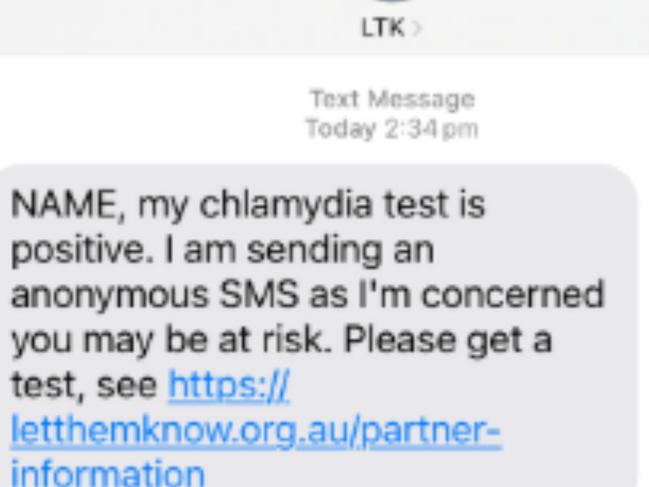
Your doctor will also talk to you about informing current and previous sexual contacts. Generally we ask people to inform contacts themselves, but you can ask your doctor to help you with this without revealing your identity. You can also use a website called letthemknow.org.au to send an anonymous text. I sent myself a test text and this is what the recipient receives:
You can get tested via your GP, a sexual health clinic or Aboriginal community health services. For younger patients I always double check contact details because sometimes the phone number on file is still their parent’s from years ago!
Young people also have the right to confidential care.

From about age 14, teens can consent to simple health care if we consider them a mature minor. We assess their ability to understand their health problem, the consequences of different treatment choices and any potential risks from procedures or interventions. From age 16, they have the same rights as adults in most situations. Health professionals will only contact a parent or carer in special circumstances like concern about risk of harm to themselves or others.
Health independence matters. From age 14, a young person can manage their own My Health Record and who has access to it. From age 15, they can apply for their own Medicare card (sometimes younger, by request).
Sexual health is just another part of staying well. So don’t wait for symptoms. Be proactive, get tested, and encourage your partners to do the same.
Dr Kavya Chaganti is a GP-obstetrician, while her husband Dr Raja Chaganti is a medical oncologist. They are also parents who are based in Sydney and have the popular Instagram @twoaussiedoctors.
More Coverage
Originally published as Kavya Chaganti: I’ve seen a drop in patients coming in for STI checks




