X-ray-guided surgery techniques exposing health professionals to radiation in Australian hospitals
Health professionals are unknowingly being exposed to high levels of radiation, putting them at greater risk of brain cancer and fertility issues. See why.
Pioneering X-ray-guided surgery techniques are exposing nurses and surgeons to radiation levels on par with uranium mining.
Operations are now frequently carried out with live X-ray images beamed into the theatre, meaning nurses, surgeons, radiologists and anaesthetists are accruing radiation exposure over time.
Every major hospital in Australia is home to at least one of the so-called Cath labs, carrying out mildly-invasive procedures, such as fluoroscopies.
The labs are also in regional hubs like Coffs Harbour and Wollongong, in NSW, and Mackay, in Queensland.
Medical radiation exposure specialist Glenn Ison said doctors had gone from doing a “handful of complex procedures to thousands” in their careers.
“When I started doing this, imaging was mostly diagnostic. We took imagery to find problems,” the 33-year medical veteran said.
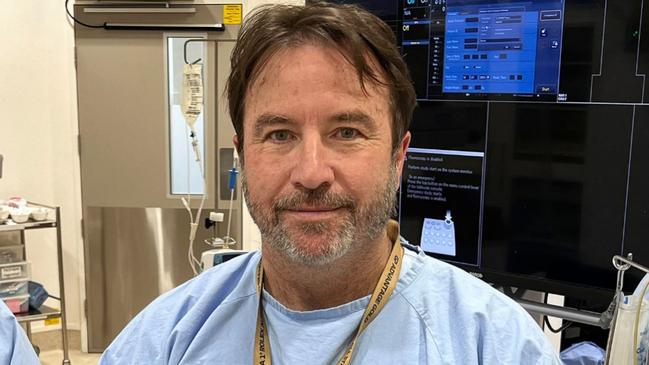
“Now we’re using X-ray guided therapy to fix problems.”
The Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) estimates the average person’s natural radiation exposure at the equivalent of 75 chest X-rays a year.
Cardiologists are exposed to the equivalent of between 2500 to 10,000 chest X-rays across a career, according to journal Cath Lab Digest.
Cath lab developer Chad Wilhelm said the theatre’s benefits were great but more safety protocols were needed by the hospitals running them.
“We have to change the way that organisations think about what is a safe environment,” the Wilhelm Integrated Solutions Managing Director said.
“I’ve had doctors pull up their pant leg and show me that they have no hair on their left side.”
ARPANSA said the exposure for some nuclear medicine practitioners was at best on par with a uranium miner and, at worst, nearly double.
The average uranium miner in Australia faces the exposure of more than 150 chest X-rays annually.
Radiation cell damage can lead to brain cancer tumours. It also raises the risk of infertility and cataracts.
A small study by the American Journal of Epidemiology found radiologists died from brain tumours at three times the rate of other medical professions.
“It is the responsibility of employers such as hospitals to ensure appropriate protection measures are in place,” an ARPANSA spokesperson said.

“The vast majority of workers in facilities that utilise radiation typically receive no occupational exposure.”
The College of Radiologists said that Cath lab staff were held to “as low as reasonably possible principles” to reduce exposure.
Some Australian hospitals, such as Brisbane’s Prince Charles Hospital, have installed new radiation protections in response.
PPE includes leaded aprons and goggles.
However, their weight leaves constant physical pressure on wearers and has been linked to orthopaedic injuries.
Cath lab workers suffer orthopaedic injuries up to seven times more frequently than other medical professionals.
“As a specialist I’ve often walked in the room and people have on the wrong lead gowns, they don’t have lead glasses, and they’re standing too close to the machine,” endovascular surgeon Nicole Organ said.
“We all know the basics of radiation safety and how to improve it. But when we’re concentrating on patient care, and trying to give the patients the best possible outcome, it’s easy to ignore.”
Originally published as X-ray-guided surgery techniques exposing health professionals to radiation in Australian hospitals





