Teen family’s help to fight rare eating disorder treatment
Lily Everson lives with a constant feeling of seasickness-like nausea, little to no appetite, regular bouts of vomiting for no reason and sensory issues relating to food textures, colours and smell.

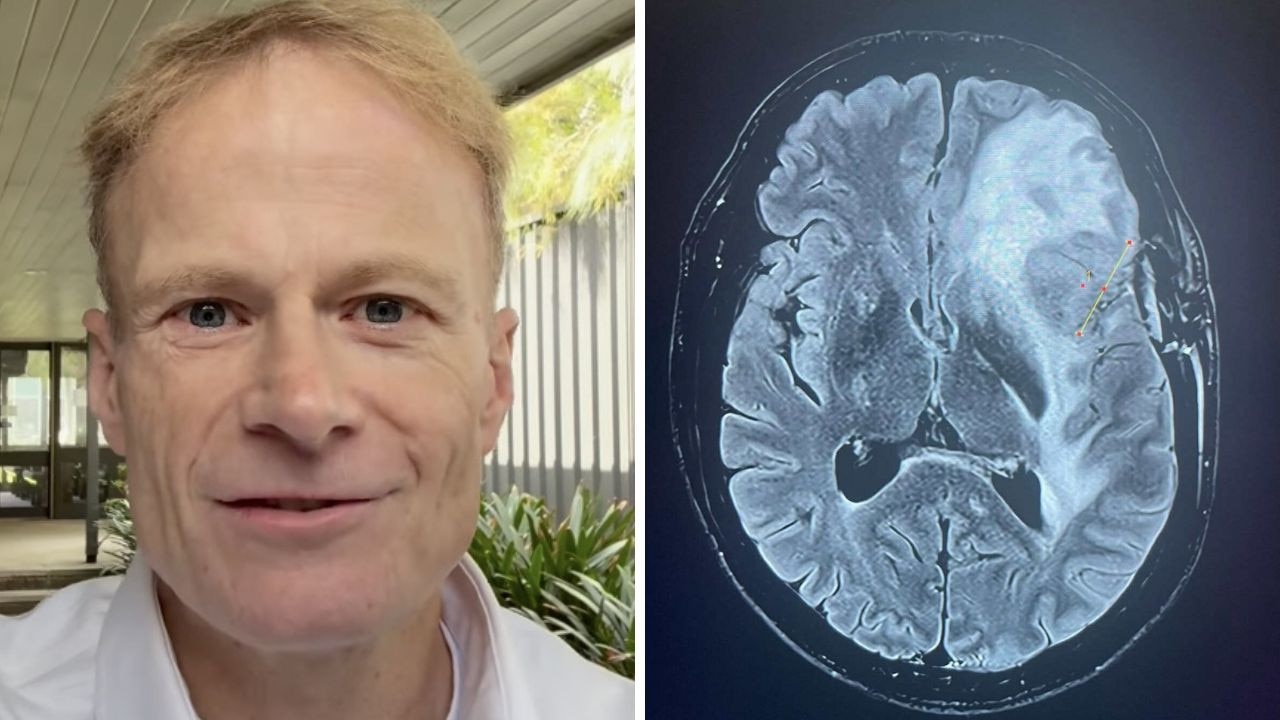
A lesser-known and crippling eating disorder has caused a Sunshine Coast teenager to dropout of school and led to an emergency hospitalisation after her appetite disappeared.
Her family is also being forced to fundraise because Medicare does not cover ongoing treatment.
Twin Waters 17-year-old Lily Everson lives with a constant feeling of seasickness-like nausea, little to no appetite, regular bouts of vomiting for no reason and sensory issues relating to food textures, colours and smell.
Her condition is called Avoidant Restrictive Food Intake Disorder.
It was exacerbated by pain caused by endometriosis, which led to surgery.
Before her health decline, Lily was a keen roller derby participant.
The teenager has stopped going to high school because of the vomiting associated with her condition and has lost 20kg since 2020.

Her complete loss of appetite, which meant she stopped eating, led to her emergency hospitalisation at the Sunshine Coast University Hospital about two weeks ago.
There, she underwent a gruelling program of force feeding through a tube inserted through her nose into her stomach.
Lily’s mother Krishna Everson said it was hard to watch.
“I have to keep reminding myself that it’s Lily’s journey and you try and step back because you don’t want to exacerbate the situation by giving advice,” Ms Everson said.

“It’s difficult to step back when you see your child powerless but at the end of the day they have to find their power.”
Back at a more healthy weight, Lily was discharged from the hospital and Ms Everson started looking for support services for her daughter.

She quickly realised that Lily’s eating disorder did not fit the mould for many eating disorder services and the only avenue available to continue treatment were private psychologist sessions costing $235 a week.
“Buying foods that are suitable are quite expensive, I’m just trying to find anything that she’ll have an appetite for,” Mrs Everson said.

The mum, a medical administration worker, is determined to continue her daughter’s treatment and has set up a GoFundMe to help with the costs, which has so far raised more than $2000.
Avoidant Restrictive Food Intake Disorder explained
University of Queensland PhD candidate Megan Bray said people with the eating disorder had to pay privately for treatment because it was not recognised under Medicare’s eating disorder treatment plan.
“Treatment is long and intense and it can cost many thousands of dollars,” she said.
The dietitian, with a special interest in eating disorders, said ARFID was one of the least common eating disorders and it occurred in about one in 300 Australians.
“Part of that is contributed to by the fact it’s under-diagnosed and under-recognised,” Ms Bray said.
She said it was not like other eating disorders that had a core focus on body image.
“Ultimately it’s this inability to meet your body’s needs or eat enough food, mostly related to sensory issues, or being worried about nausea or vomiting,” the dietitian said.
The dietitian said it was “so much more” than picky eating.
“There’ll be such a limited amount of foods they’ll eat, it’s not uncommon to meet someone who will only eat five foods,” Ms Bray said.
“They might need a specific brand of that food.
“The other part that would flag ARFID is if they’re losing lots of weight or a child is not staying on their growth trajectory.”
The dietitian said changes needed to occur to better recognise the condition.
“I would like to see it recognised and funded under Medicare’s eating disorder treatment plan,” she said.
“I think people in the sector are aware of this and that the needs of people with ARFID are not being met and there’s a genuine push to have ARFID recognised.”
Psychologist’s perspective
Sunshine Coast clinical psychologist Vera Keatley said people with ARFID may be offered 10 sessions with a psychologist under a mental health plan to treat the condition.
She said it often took more than 10 sessions to treat the eating disorder.
Ms Keatley said, under an eating disorder management plan, people were offered up to 40 sessions with a psychologist and 20 sessions with a dietitian.
“If you have a diagnosis of anorexia you’re straight in, bulimia or binge eating you have to score a certain number on a questionnaire, but the questionnaire is not about ARFID so it’s not fair,” Ms Keatley said.
The clinical psychologist said sensory sensitivities could lead to the eating disorder, as could a food trauma like choking.
Low or no appetite and no pleasure in eating may also lead to the condition.
The clinical psychologist also said a study showed 71 per cent of those with the eating disorder were not underweight, but they were not meeting their nutritional requirements.
This may lead to not enough nourishment to build bones and grow, diabetes, fatigue, poor self esteem, family time meal conflict, peer isolation and more, she said.
How to help Lily
Lily’s dad has also organised a crossfit event on September 16 to raise funds for his daughter’s treatment.
Search Level Up for Lily on Facebook for more details.
The link to the GoFundMe for Lily is here.
More Coverage
Originally published as Teen family’s help to fight rare eating disorder treatment