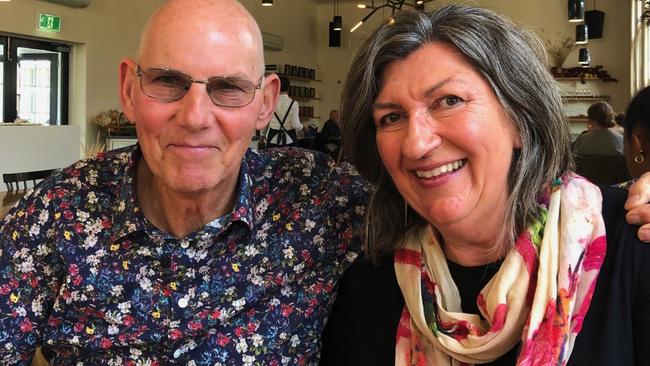
John Street uses Tasmania’s new VAD laws for a “calm death”
“I sat with him while he took the substance and he was relieved and calm as he relaxed into sleep”: When John Street decided he would end his life via voluntary assisted dying, his wife was grateful he could go in peace.
Tasmania
Don't miss out on the headlines from Tasmania. Followed categories will be added to My News.
Always fit and healthy, John Street never thought he’d need help to die.
Even after being diagnosed with stage 4 colorectal cancer in September 2021, the 71-year-old retiree was strong and well and still cycling and gardening.
But when the cancer mutated, and he was put in palliative care, Mr Street decided he wanted to die at home and use Tasmania’s new voluntary assisted dying (VAD) laws.
His wife Mary-Kate Pickett says she is grateful that VAD was available and has nothing but praise for everyone involved in the process.
“The care we both received from all of the professionals was respectful and kind,” Ms Pickett said.
“Both of us saw the availability of VAD as an important part of John’s cancer journey and it was his preferred way to end that journey.
“This is what he had wanted and the alternative of more illness and helplessness was simply not an option for him.
“While it may not be suitable for everyone who might be eligible, having the option for a calm death at a time of his own choosing was very much John’s way, making his own decisions and taking control of his own situation.”

The couple moved from New South Wales to a property near Cygnet and while he had no symptoms, a positive bowel screening test and follow-up colonoscopy identified his cancer.
In February 2022, he was given six to nine months to live.
However, by early 2023, Ms Pickett said he had started “experiencing high levels of pain, and was feeling very unwell”.
“He had lost weight and had no appetite. He went into the palliative care ward where he was prescribed higher doses of stronger pain management.
“At this stage, John realised that he was not going to get better, and that he was getting closer to dying.
“He had always wanted to die at home, so the plan when he went into the palliative care ward was to set up a medication regime that could be managed at home.
“When John came home from hospital, he contacted the navigator at the Voluntary Assisted Dying Commission to make enquiries about the process, and to start the steps required for VAD.
“The navigator was professional and caring.
“Before his diagnosis, and even for a while afterwards, he felt so strong and healthy that he simply didn’t consider it as something he would need.”
In the last three months of his life, Mr Street’s pain was “significant”.
“While the medication he was on eased his pain, it also caused him to be drowsy or nauseous and he was never completely pain free.
“John had previously never been on any medications and would take just one panadol for a headache.”
Ms Pickett said her husband, who worked in local and state government, was “a very private person, and his pain medications caused him to have limited energy to be with people”.
“We had regular but brief visits from friends in the days leading up to the day (February 24).
“Friends and family sent emails and texts in the last couple of weeks of John’s life, with memories and kind thoughts that he appreciated.
“I sat with him while he took the substance and he was relieved and calm as he relaxed into sleep.”
16 Tasmanians voluntarily end their lives in first six months of scheme
Tasmania’s Voluntary Assisted Dying Commission is hoping to streamline its processes after doctors expressed “ongoing and significant frustration” with time-consuming documentation.
In its six-monthly report it says that the “non-patient facing work component” is in the order of six-to-eight hours per patient.
“Practitioners have, in particular, expressed frustration with the amount of duplication across forms while others have experienced difficulty complying with the Act’s documentation requirements without error,” the report said.
The Commission says it is looking at setting up a management database and portal system for health professionals.
“In the interim, work continues to streamline approved forms to remove duplication, to enable increased electronic completion and to remove the potential for error in completion,” it said.
Former emergency specialist at the Royal Hobart Hospital Dr Bryan Walpole said there were 13 forms to complete which were time consuming, “complicated” and could take up to 8 hours for documentation and visits.

He also said the terms were restrictive and “having to testify that folks have less than six months to live is awkward”.
“It’s easy when there are a few months left, but research shows doctors are poor at predicting life span.
“Over my clinical life I have heard countless times ‘the doctors gave me 3/6/12 months to live, and here I am at 80. Cancer is capricious indeed.
“The 12 months for neurological conditions is similar, look at Neale Daniher’s 10 years since his MND diagnosis.
“As the drug has a long life, I think ‘death is reasonably forseeable’, would be kinder.”
The report found 63 people had successfully completed VAD training including 30 doctors, 23 nurses and 10 pharmacists.
Sixteen Tasmanians have died in the first six months of the new laws.





