Leaked memo and data reveal top Sydney hospitals’ shock treatment of patients
Two hospitals have mothballed wards and a massive X-ray backlog and patients who’ve had mastectomies and hysterectomies will be discharged just hours after surgery, a leaked memo shows.
NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
Exclusive: Women who’ve undergone mastectomies and hysterectomies are to be pushed out of hospital beds just hours after their surgery to meet “aspirational benchmarks” for patient discharge numbers, leaked documents from NSW Health show.
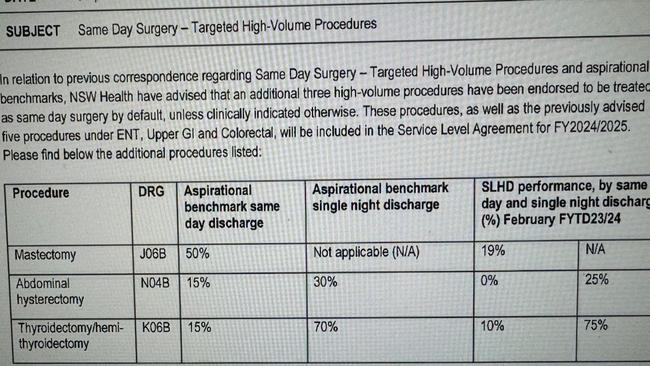
In a shocking memo, which has been widely circulated among medical staff across the Sydney Local Health District (SLHD), health administrators revealed they want high-volume procedures treated as same day surgery by “default” unless “clinically indicated otherwise”.
It states they are aiming to have at least half of all mastectomy patients – up from 19 per cent currently – out of hospital on the same day and 15 per cent of women who have had abdominal hysterectomies out – up from a current zero.
This contradicts NSW Health’s own literature advising most women will stay in hospital for 2-4 days after an abdominal hysterectomy.
The Australian Medical Association’s (AMA) NSW branch has expressed concern patients discharged within hours of major surgery can face complications and many return for follow-ups, complaining of trying to self-manage pain, nausea, vomiting and difficulty mobilising.
AMA Councillor and general surgeon Dr Fred Betros said “I know there’s no way I’d let one of my family be managed that way”.
“There’s no good data to support this approach … and I consider it fraught with risk for the patient, the clinical staff and the organisations,” said Dr Betros.

A spokesman for NSW Health said eligibility for day surgery is determined using a thorough screening process by a multidisciplinary clinical team. All day surgery patients are provided with comprehensive pre-surgery and follow up care to ensure they are supported before, during and after their stay in hospital.
The revelations come as hospitals including Concord and Royal Prince Alfred (RPA) face increasing concerns over a lack of nursing staff, mothballed wards and a massive X-ray backlog and new X-ray tool.
The Assistant General Secretary of the NSW Nurses and Midwives’ Association, (NSWNMA), Michael Whaites, said they were aware of staffing and workplace issues at RPA and held concerns that temporary contracts were not being renewed or were being terminated early.
“This has a significant impact on the hospital workforce, which is already struggling with staffing shortages, “said Mr Whaites.

“We understand some of the roles that have been affected are Clinical Nurse Consultant (CNC) and Clinical Nurse Educator positions.
Mr Whaites said they play a crucial role and are specialists in their field, making them some of the most experienced nurses in the workforce.
“They provide comprehensive continuity of care to ensure positive patient outcomes,” he said.
The Association has also raised concerns about cuts to CNE’s who are vital to providing clinical support to new graduates.
“We understand after-hours CNE positions are being reduced, some CNEs are not being replaced when they’re on leave and some are being required to take on a patient load, rather than perform their education role.

“We are deeply concerned by this. Given the large intake of new graduates into the public health system this year, which we welcome, we should be seeing an increase in CNEs, not cuts.
“Clinical Nurse Educators and Clinical Midwifery Educators provide education and clinical support to the entire workforce. Positions like this should be seen as crucial in retaining and supporting our existing workforce and in preventing the loss of junior and experienced staff as a result of burnout.”

It comes as it’s revealed NSW Health has implemented a new “Medical Imaging Prioritisation Tool” dictating the more than two year backlog of X-rays across the hospitals should not be reported on unless absolutely necessary.
The decision comes as NSW Health tries to slash X-ray queues, which has previously peaked at 200,000 a decade ago – a figure health officials promised would never happen again.
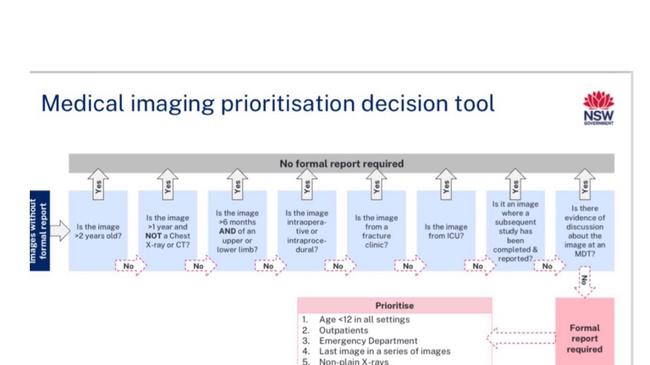
But doctors warn early cancers could be missed and this shouldn’t be allowed to happen.
The AMA NSW said it was indicative of the monumental resourcing abyss that is ever-widening in NSW.
Dr Betros said “we are not aware of this imaging prioritising tool but if it is being put into action, it is purely due to a resourcing and financial issue and … Health must bear complete responsibility for any adverse outcome …”

The President of the Royal Australian and New Zealand College of Radiologists, Professor John Slavotinek, said he long-term solution to reducing scanning backlogs in our public hospital system is to ensure an adequate workforce.
“It is therefore important that there are enough training places for junior doctors to secure the next generation of radiologists,” said Professor Slavotinek.
A spokesman for the SLHD said the tool will not apply to images taken after mid-January and clinicians directly involved in the care patients will already have reviewed the images.
“The tool helps identify older medical images where formal radiologist reporting is
appropriate and has been designed to specifically minimise the risk of undetected cancers
being missed,” the spokesman said.
The use of the medical imaging prioritisation tool is not a cost-saving measure. It will
support SLHD’s clinicians as they continue to provide safe, high quality, and timely care to
the community.”
More Coverage
Originally published as Leaked memo and data reveal top Sydney hospitals’ shock treatment of patients





