IVF treatment breakthroughs to create miracle babies
Experts are in a race against time to find ways to improve the success rate of IVF to help Australian women create healthy embryos.
Parenting
Don't miss out on the headlines from Parenting. Followed categories will be added to My News.
As IVF success rates flatten out the research race is on to find new ways of improving the number of live births from fertility treatment.
Using technology to identify the best embryos, making a woman’s womb more hospitable for a pregnancy, artificial intelligence and looking at bacteria and viruses are key areas being explored.
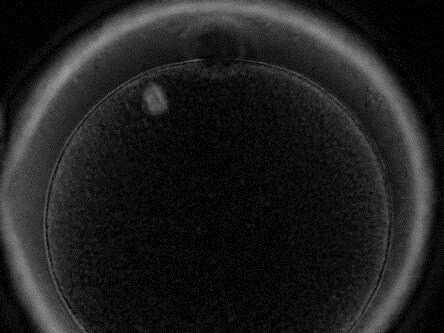
Director of Clinical Research of IVF Australia Dr Christos Venetis is using polarised light microscopy to select the eggs most likely to develop into a healthy embryo.
His study, recently published in Fertility and Sterility Journal, shows for the first time that the type of meiotic spindle of the egg, as seen using non-invasive polarised light microscopy, can help predict the probability of individual eggs forming into a normal embryo.
“This technology could have important applications in the future in the way we select the best day 5/6 embryo for transfer and hopefully shorten the time to pregnancy for patients,” he said.
It could also help women understand if they needed to have more than one egg collection.
If only two of the 10 eggs collected in one cycle had normal meiotic spindles a woman might opt to have another egg freezing cycle but if 8 of the 10 eggs were normal this may not be necessary, Dr Venetis said.
Professor Michael Chapman from IVF Australia said polarised light microscopy is currently being used in IVF Australia on patients who had failed cycles and costs around $300.
The clinic was planning to run a trial in Sydney later this year to test whether it made a difference in IVF outcomes.
The clinic has also separately begun testing artificial intelligence and time lapse photography, photographing a developing embryo every 15 minutes over five days to check rate of the division of cells.
By day five, there should 200-300 cells in the developing embryo, a signal that it is a good embryo.

IVF Australia has fed one million time lapse photos of these developing embryos into a maxi computer and told it which ones led to a pregnancy and which ones did not.
“We use it routinely in the lab to give a score as to which embryo is best to put back and it appears to point to a 4-5 per cent increase in pregnancy rates,” he said.
Genetic testing of embryos was another way of improving pregnancy rates.
In the US, 90 per cent of embryos are genetically tested but in Australia it’s just 15 per cent.
This type of testing costs $700 per embryo and is not economic if you only have a small number of eggs and questions remain over its accuracy, Professor Chapman said.
Professor Luk Rombauts from Monash IVF said one crucial key to a successful pregnancy was a healthy and receptive womb in the mother.
“At the Hudson Institute we are looking at particular markers for receptivity in the lining of the womb – it’s like a Teflon molecule that makes the lining too slippery so the embryo can’t attach,” he said.
“There are a number of ways we could reduce the expression of this molecule,” he said.

MUM GOES THROUGH EIGHT IVF CYCLES
Maximus turns three today but it’s been a long journey for his parents Angelina and Peter who went through eight cycles of IVF to get pregnant.
Angelina, a 38-year-old administration worker, tried for two years to get pregnant naturally before starting IVF treatment at the age of 34.
And it took a technological breakthrough to find the right egg that finally gave her a baby.
Testing showed her eggs were not good quality and she was not producing enough.
“I only got one egg from my first harvest and collections varied from 0-8,” she said.
“Only one or two would survive to last the transfer period and none of them were able to be frozen,” she said.
On her eighth cycle there were two eggs left and her fertility specialist Dr Manny Mangat at IVF Australia used polarised light technology to look inside Angelina’s eggs to observe the meiotic spindle.

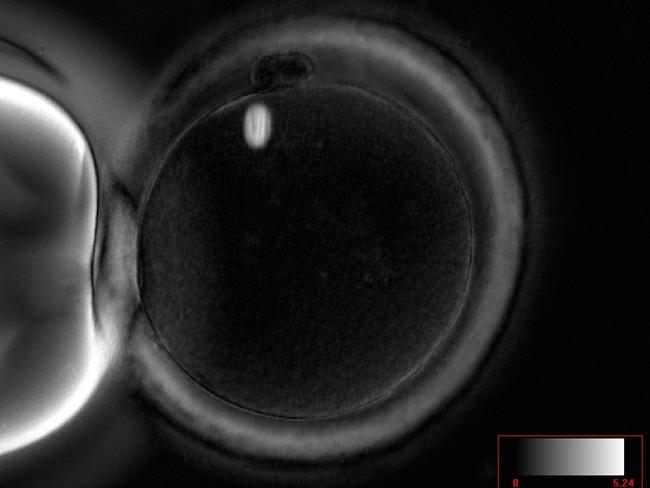
Eggs with normal spindles are more likely to be fertilised and develop into a healthy embryos.
“We used polarised light to pick the better of the two and the other one didn’t survive,” she said.
The surviving egg took and Angelina gave birth to her “miracle” baby boy Maximus.
“So many women struggle to fall pregnant and research comes along and the process helps women so much,” she said.
A planned new website that would allow couples to compare the success rates of IVF clinics was a welcome development, she said.
“Honestly we were a little slack and didn’t look at success rates, it was only when we were struggling to fall pregnant we looked at other places but we stuck with IVF Australia,” she said.
Angelina says it’s great to be a mum.
“I’m so grateful. He’s a crazy boy, full of energy and he loves playing and getting into mischief,” she said.
MORE NEWS
Cost of IVF slashed for thousands of women in NSW
New tool to help IVF mums conceive
The hidden costs in your health fund
The disease set to become Australia’s biggest killer
AUSSIE EGG DONORS GO UNPAID
Infertile Australian couples are being forced to go overseas to obtain donor eggs because unlike the US and Europe we don’t pay egg donors and demand is outstripping supply.
Fertility Society Australia president Professor Luk Rombauts told News Corp the recruitment of donors has not kept pace with demand.
And there had been increased demand after the legalisation of gay marriage, he said.
IVF Australia’s Professor Michael Chapman said he was sending “a patient a month overseas to find donor eggs”.
“The Spanish have the highest number of egg donors in the world because they pay donors $1500,” he said.
“For a university student for two weeks of injections and an egg collection that could be tempting,” he said.
The United States also pay donors up to $5,000 for their eggs with some couples advertising on social media they are prepared to pay $40,000 to egg donors.
Professor Chapman says Australia has an inherent philosophy about medical donations such as blood and organ donation being altruistic.
Two reviews into Australia’s altruistic system argued against making any change that would allow payment for donated eggs, he said.
Originally published as IVF treatment breakthroughs to create miracle babies


