Doctors, health workers prepared to take on extra roles to reduce dependence on NSW psychiatrists
Doctors and health workers say they are prepared to take on extra roles to reduce the dependence on psychiatrists, under the state government’s plans to reform the mental health system.

NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
Doctors and health workers say they are prepared to take on extra roles to reduce the dependence on psychiatrists, under the Minns government’s plans to reform the mental health system.
The Daily Telegraph can reveal thousands of healthcare professionals will replace psychiatrists in prescribing medications, diagnosing conditions and developing treatment plans, as psychiatrists threaten to resign from the state’s hospitals in pursuit of higher wages.
The government confirmed more than 5600 nurses could already manage stages of care including diagnoses and recovery, while up to 2000 psychologists, occupational therapists and social workers could oversee case management and therapy.
NSW Mental Health Minister Rose Jackson said health workers were trained and ready to take on greater roles in the mental health system.
“This is not about asking anyone to do anything they aren’t trained or qualified to do, this is about ensuring we have a resilient mental health system that can provide the best care possible,” Ms Jackson said.

“This is about long-term reform so that no single healthcare specialist can hold the entire system to ransom.”
Under the reform plans, psychiatrists would be freed up to perform jobs only they can perform, such as electroconvulsive therapy, through training and recredentialing other workforces to take on additional duties – with the process already under way in local health districts impacted by psychiatrist shortages.
Royal Australian College of General Practitioners NSW chair Rebekah Hoffman said general practitioners could treat conditions such as attention deficit hyperactivity disorder but must wait for “middleman” psychiatrists to confirm diagnoses and prescriptions, which could take years in regional areas.
“Both GPs and patients are frustrated,” Dr Hoffman said.
“They don’t understand why it takes seeing someone else and spending a large amount of money to get the initial diagnosis and script.”
Sydney peer worker Kylie Smith, 41, also welcomed more support opportunities, having spent 13 years helping others through suicidal ideation.
“This is a long time coming,” she said.
“There is a real need for peer workers who have that lived experience to have a seat at the table … there needs to be a more holistic approach.”
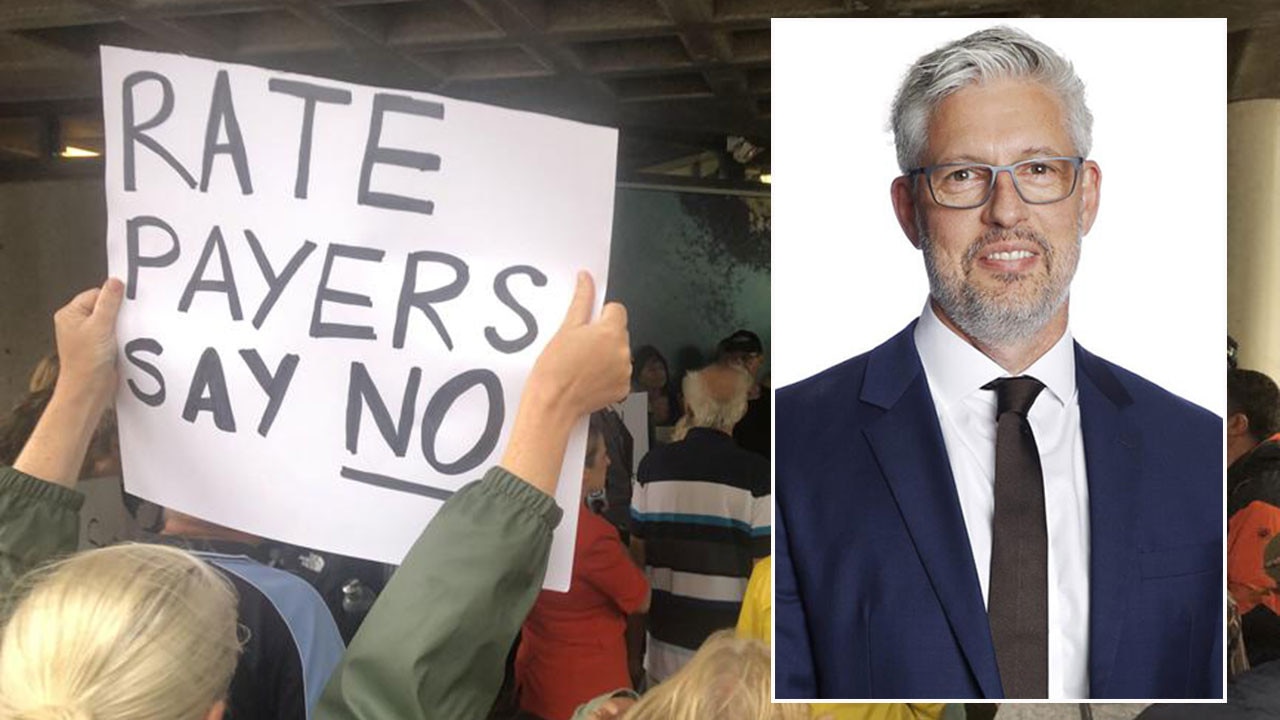
With more than 100 psychiatrists threatening to resign in the next two weeks, Health Services Union NSW secretary Gerard Hayes said “every crisis was an opportunity”.
“For too long, the delivery of mental health treatment in NSW hospitals has resembled a feudal system where psychiatrists sit at the top of the tree,” he said.
“This reform is beyond overdue … the best way to preserve universal health care is to allow the broader workforce to use all their skills and ensure tax payers get maximum value.”
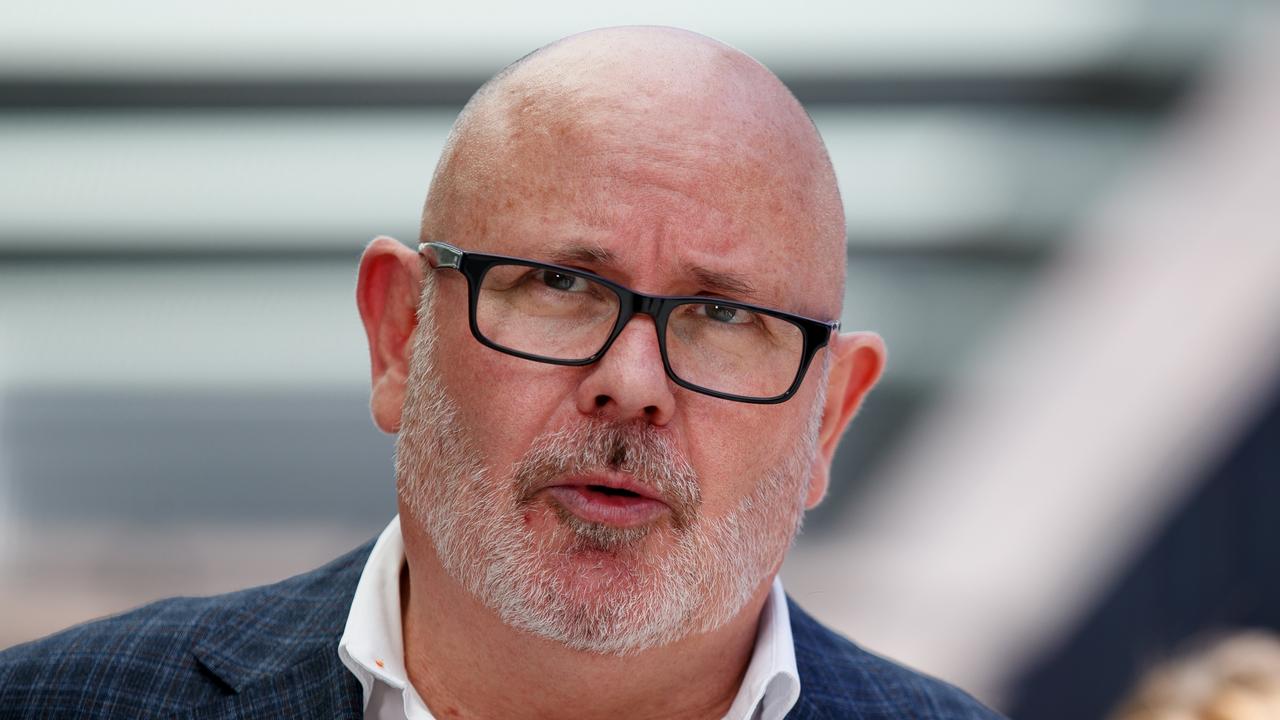
Speaking on behalf of psychiatrists, Australian Salaried Medical Officers Federation executive director Andrew Holland said the plans would lead to burnout and mistakes.
“It’s simply not appropriate to ask doctors, nurses, or allied health professionals to take on the duties of psychiatrists,” he said.
“Real reform starts with retaining and supporting psychiatrists, not replacing them with professionals who lack the necessary training and experience for the role.”
Originally published as Doctors, health workers prepared to take on extra roles to reduce dependence on NSW psychiatrists