Hudson Institute’s ‘natural’ mesh offering desperate women hope
Sally Maconochie had “everything that normally holds the pelvic organs in place ripped from the bone” during childbirth. This is why she hopes she may be able to run again.
Conditions
Don't miss out on the headlines from Conditions. Followed categories will be added to My News.
A “natural” 3D mesh that could be customised to treat women with pelvic organ prolapse has been developed by Australian researchers.
Pelvic organ prolapse (POP) is a debilitating gynaecological condition that affects around one in four women, usually following childbirth.
In a world-first the team from the Hudson Institute fabricated degradable meshes they hope cannot only help naturally repair the damage caused by POP, but also give desperate women “real hope”.
The team expects to start clinical trials within two years.
POP is essentially a hernia where tissues, pelvic floor muscles and supporting ligaments are injured causing the organs to protrude outside the body.
It can be exacerbated by age, ethnicity, multiple births, obesity and family genetics and around one in five women will require surgery.
Previously it was treated using a synthetic polypropylene mesh, but this method was banned in Australia in 2017 following serious medical complications that led to class actions, including in Australia.
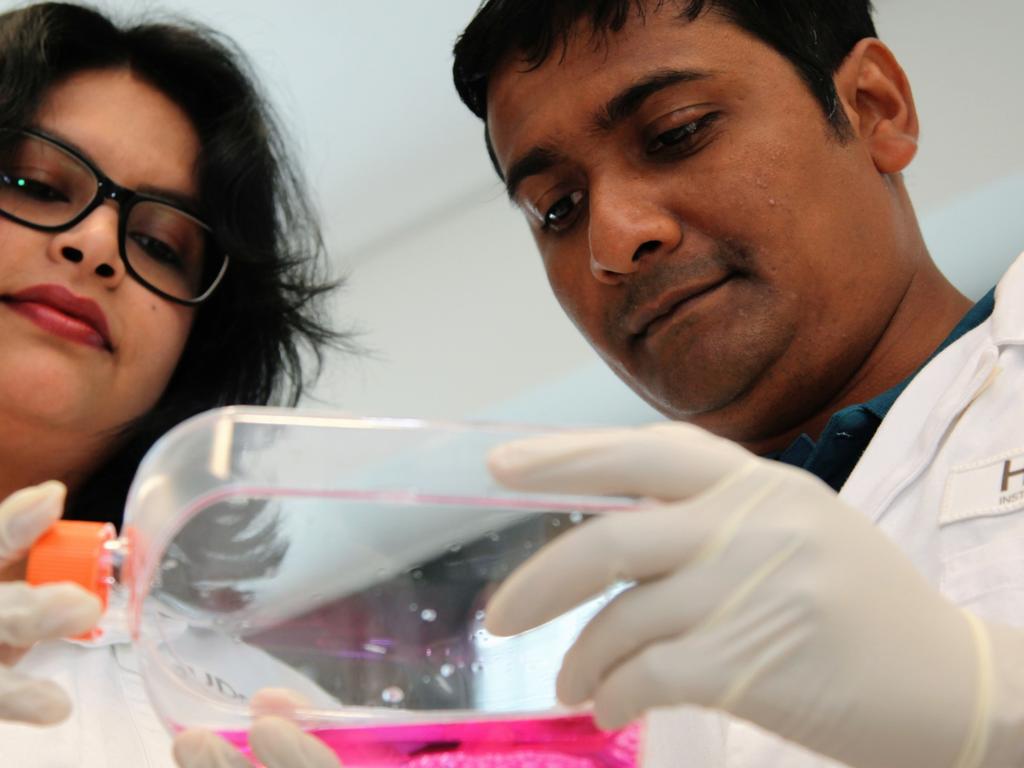
Now the Hudson Institute researchers hope their alternative degradable and compatible mesh may be used by surgeons to tailor repairs of the pelvic floor and when its job is done, the mesh will be reabsorbed naturally.
Dr Kallyanashis Paul and Associate Professor Shayanti Mukherjee from the Hudson Institute fabricated the meshes using advanced 3D printing.
The authors say Dr Paul’s specialist knowledge of this technology was key to the success of the project, the results of which were published in the Advanced Science journal.
“Current treatments normally include some conservative approaches like pelvic floor muscle exercise or pelvic floor training sessions,” Dr Paul said.
“But they can be a temporary solution and most women will need surgical solutions in the end.”
He said the team was re-engineering the mesh using a different kind of technology.
“Our hypothesis is that cells would be attracted to the mesh and deposit collagen to form a matrix around it to help repair the pelvic floor.”
Associate Professor Mukherjee said the team’s latest study provides hope, “by developing meshes that can boost native tissue repair, so the body will eventually reabsorb the mesh, leaving healthy new tissue and reversing the damage that POP can cause.”
They said they used preclinical models to test design factors required to make a mesh that the body will accept, not reject.
Sally’s story

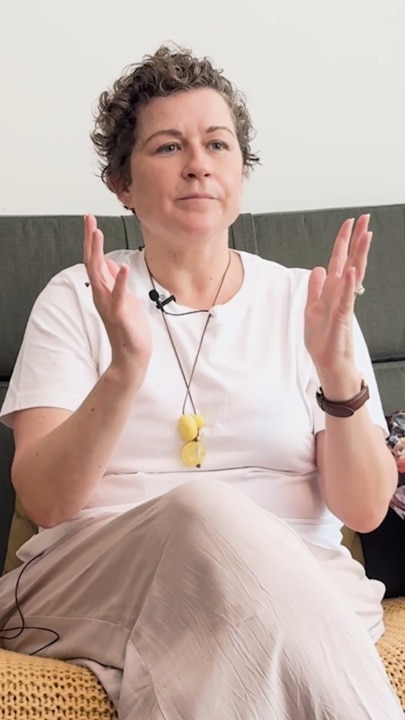
For mum of one Sally Maconochie success of this mesh would, she said, be a godsend.
Ms Maconochie, 43, said POP impacted every aspect of her life, every day.
She was diagnosed with the condition following the traumatic birth of her son eight years ago, but knows now that there were significant factors that also put her at risk.
“I was unaware that family history played a part,” Ms Maconochie said.
“About a year after I got my diagnosis my mum told me that she also had a prolapse and my grandmother did as well.
“But you know the way of the Boomers is not to talk about these things and with prolapse people don’t talk about it, even now.”
Ms Maconochie said while her condition limits her physically, “I still have a voice and I can talk to people about this.”
Knowledge is key for women.
Ms Maconochie said if she had been aware of the risks associated with developing POP, including traumatic birth and family history, she would have taken more ownership of childbirth and opted to have a caesarean birth.
Ms Maconochie was also diagnosed with bilateral levator avulsion, the traumatic separation of muscle from the pelvic bone, after her son’s birth.
“Not only did I have a prolapse, but everything that normally holds the pelvic organs in place had been ripped from the bone during childbirth,” she said.
“The only thing that can put the muscle back onto bone is mesh, which is why I am closely following this one developed at the Hudson Institute.”
The former marathon runner says she is now severely limited physically because of the condition.

“I have to be really careful about every day; how much I’m on my feet, how much I’m sitting down or lying down,” she said.
“Everything is managed in terms of my bowels and what I eat and how I move and what I do.
“I can’t exercise more than a weekly yoga class because I can’t have any intra-abdominal pressure.
“And while I could have more children, we made the very difficult decision not to because of this and that was the hardest decision of them all.”
Ms Maconochie is now counting on the success of the clinical trials of the new mesh.
“If we can get these trials happening, it would change my life.”
Tips from the expert - pelvic floor physiotherapist Janetta Webb

If you have symptoms, don’t ignore them. It’s better to get checked out early to prevent worsening.
Symptoms of prolapse could include vaginal heaviness, dragging or a bulge, leakage or difficulty emptying your bladder or bowel, discomfort with sex.
Learn how to work your pelvic floor muscles correctly. One in two women may not be doing it right.
The ability to release the muscles is just as important as the ability to work them.
If you’ve tried the exercises and feel they’re not making a difference, you may need to see a physio for a tailored program
Your GP can help you find a pelvic floor physio
Exercise your pelvic floor muscles daily throughout pregnancy and after your baby’s birth, whether you have a vaginal or caesarean birth
Like all muscle training, it takes a few months for the muscles to get strong so keep going!
Continue to exercise your muscles regularly throughout your life, it’s never too late!
For more information visit the Continence Foundation of Australia or Jean Hales for Women’s Health.
More Coverage
Originally published as Hudson Institute’s ‘natural’ mesh offering desperate women hope