A surgeon, a tiny laser and a cure to blow your mind: Revolutionary epilepsy treatment
Music teacher Dawn Kenny’s seizures get so bad it’s too dangerous for her to drive. But we take you behind the scenes to show how her life could change in just 5 minutes.

Conditions
Don't miss out on the headlines from Conditions. Followed categories will be added to My News.
Just five minutes.
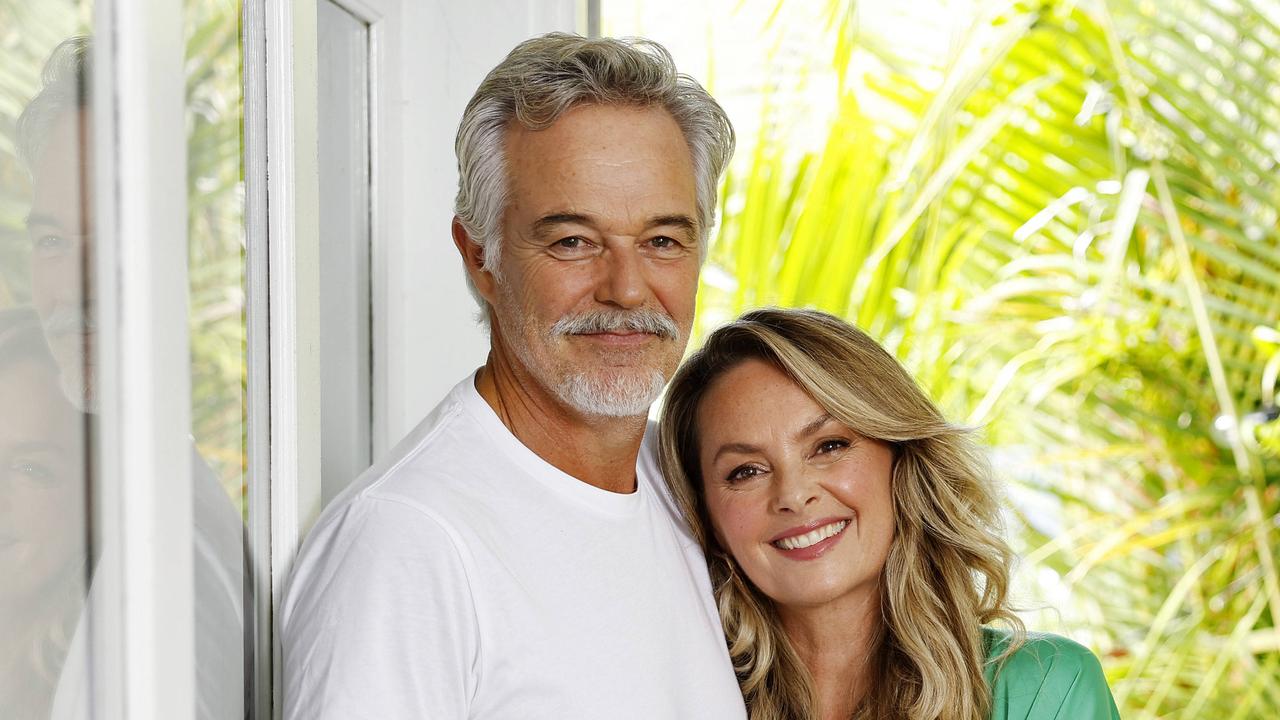
After almost 50 years of unpredictable, debilitating seizures, Dawn Kenny’s once inoperable epilepsy comes down to no more than five minutes.
That’s about how long a neurosurgeon, using a laser so tiny that it can reach into parts of the brain so hard to reach that it once rendered her condition inoperable, needs to dissolve the responsible brain tissue.

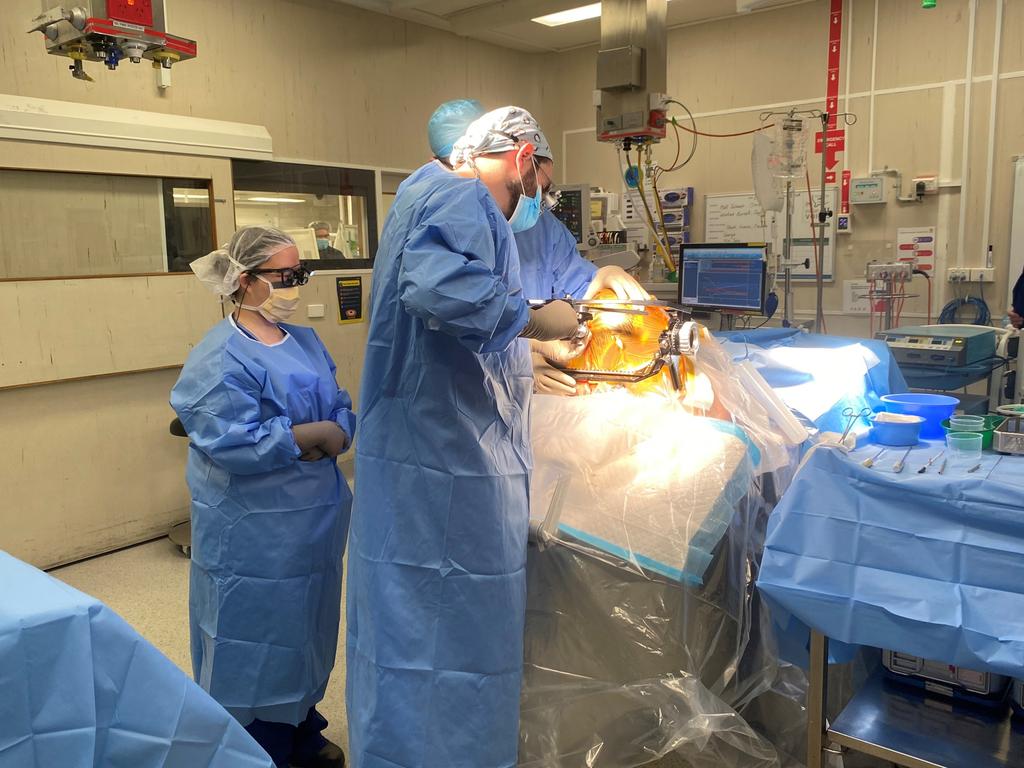
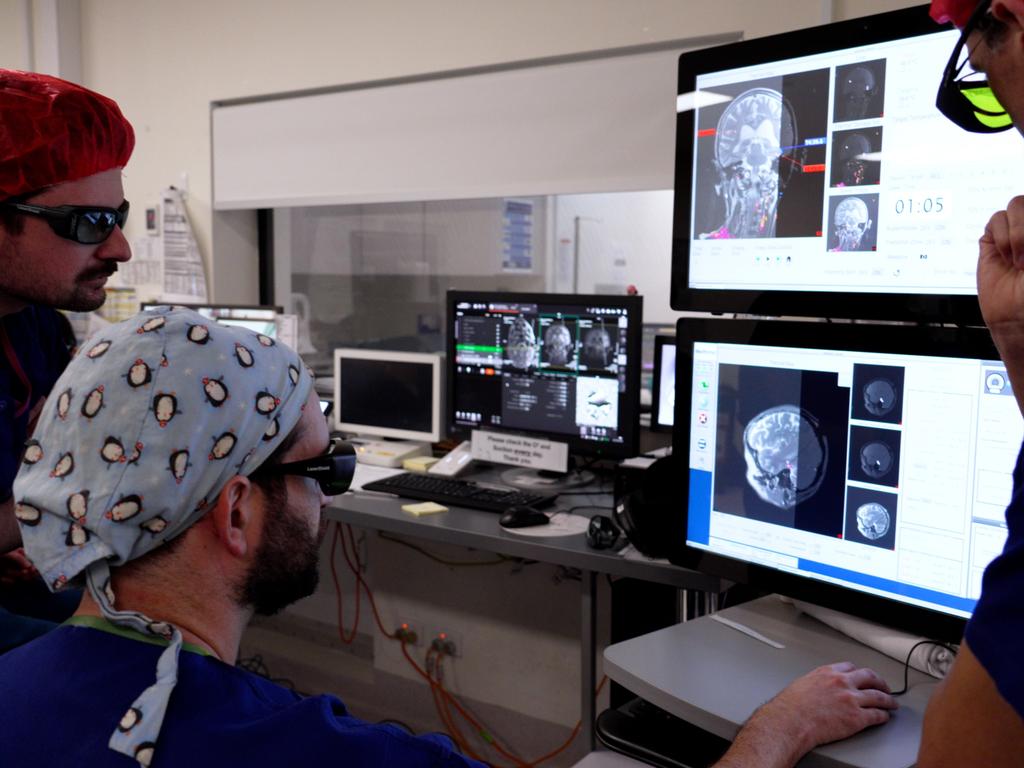
Despite the wall between him and his patient, cutting-edge neurosurgery is under way and Dr Matthew Gutman is operating deep inside his patient’s brain.
The laser, inserted earlier that morning with pinpoint accuracy, hums as flashes of colour flicker across the screen before Dr Gutman.
Staff work with a quiet, practised calm, but this is not routine surgery.
The Alfred became the first hospital in Victoria to perform this procedure – and just the second in Australia – in 2024.
And, after a successful start, the hospital is ready to take the Sunday Herald Sun behind the scenes.
Dr Gutman, the Alfred’s epilepsy surgeon lead, said giving a patient a life free from debilitating seizures was “exceptionally rewarding”.
“One of the reasons I absolutely love epilepsy surgery is because it’s one of few areas in neurosurgery where we can actually cure the patients,” he said.

This was sometimes out of reach for patients with drug-resistant, inoperable epilepsy, until a new surgery overseas, called Laser interstitial thermal therapy, started to challenge the definition of inoperable.
Spinal and neurosurgeon Dr Gutman spent five years working towards bringing LITT to Victoria.
He travelled overseas, and with the support of a Churchill Fellowship underwent several months of training in the surgery at a specialist hospital in the US.
He said, unlike traditional brain surgeon, the procedure was “minimally invasive”.
“Instead of a big, open cut … we just make a tiny, micro pilot hole in the skull,” he said.

Surgeons then use a specialised frame to carefully insert a laser fibre, with pinpoint precision, into the patient’s brain.
The patient – still under anaesthetic – is then wheeled out of theatre and carefully placed in the MRI scanner.

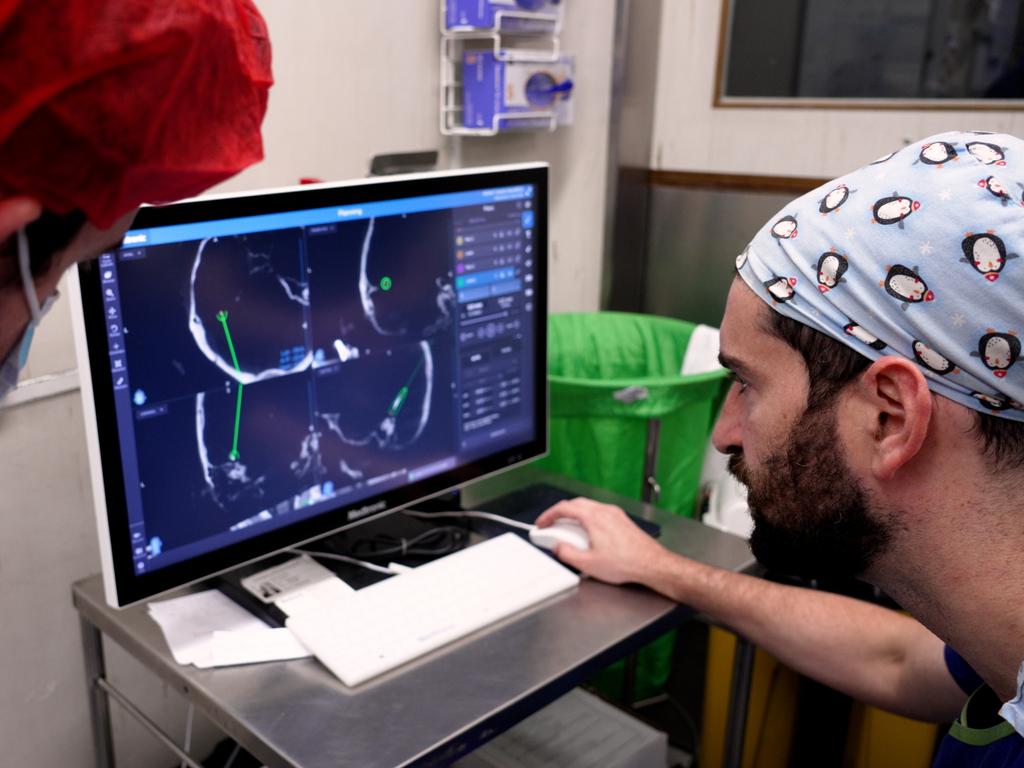
Dr Gutman can then control the laser while sitting outside the scan room, and begin the second stage of operation.
Real-time brain scans – overlaid with more detailed imaging from earlier – allow him to carefully monitor the levels of heat.
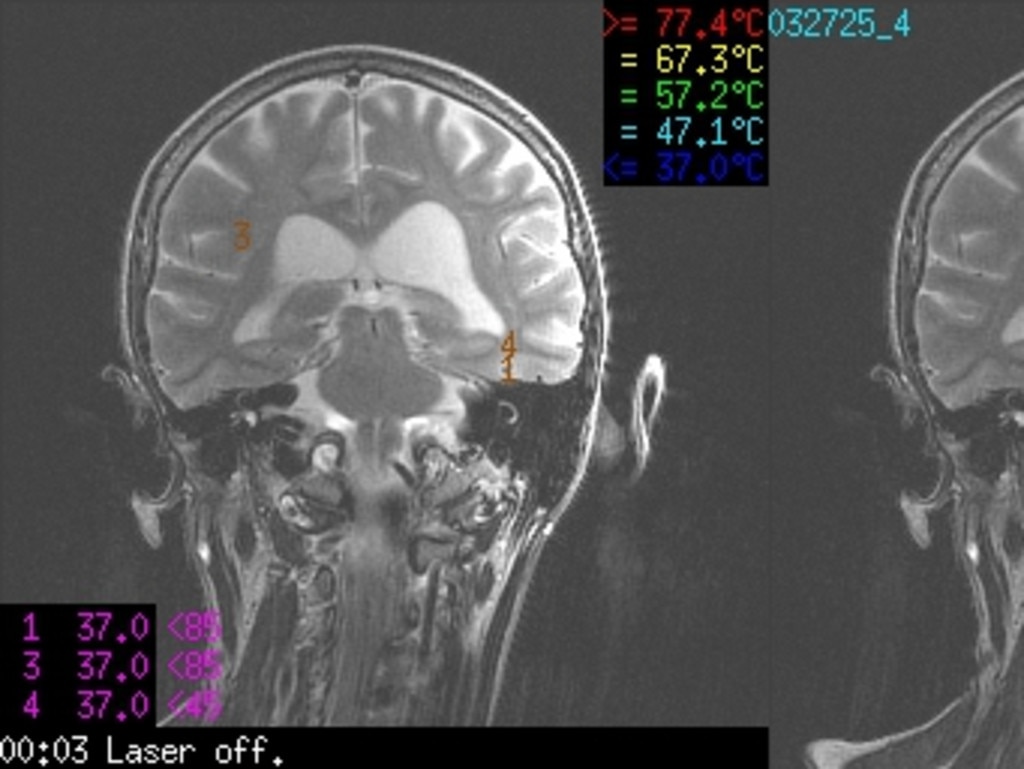
He said: “We can directly visualise in real time ourselves lesioning and destroying the part of the brain that causes the epilepsy.
“We can actually access really deep areas of the brain safely and then ablate them, and then send the person home the next day.”
The surgery can also be used to target some brain tumours.
The team performs one LITT procedure every month but hopes to secure funding to expand the program.

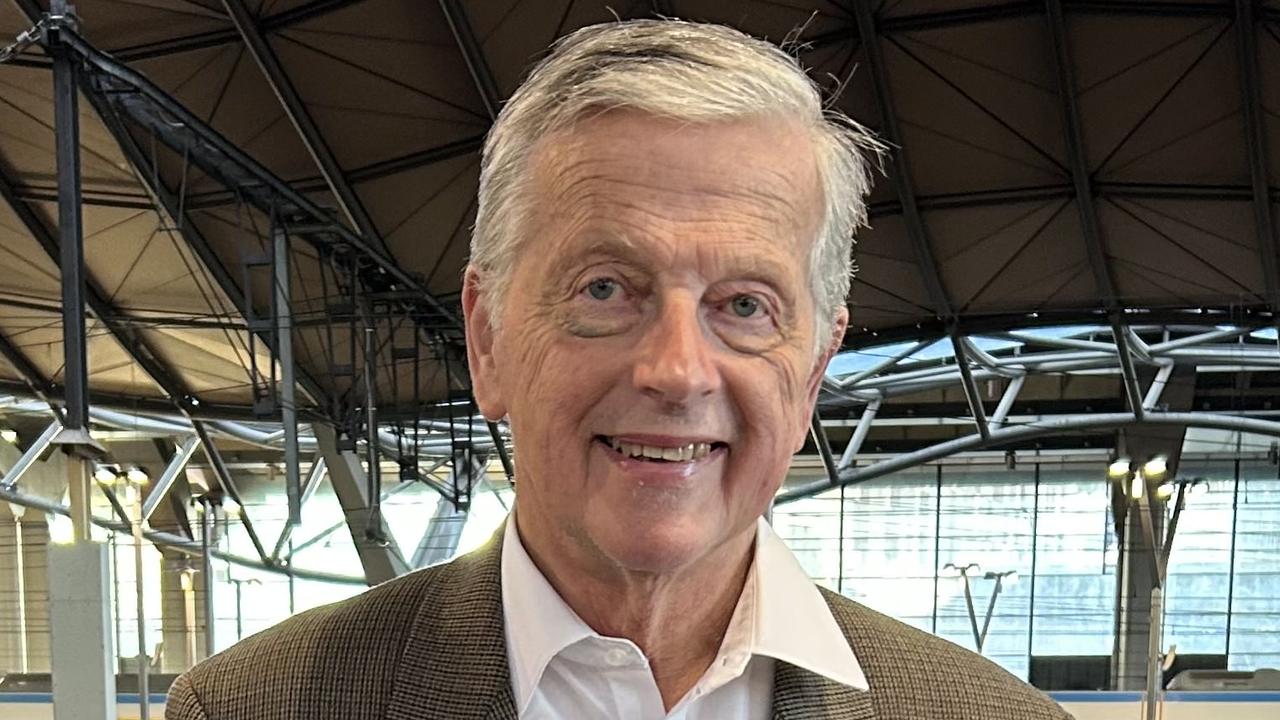
Alfred neurologist and Brain Program director Professor Terence O’Brien said about two thirds of patients responded well to anti-seizure drugs, and traditional epilepsy surgery – while very effective for the right patient – was not a suitable alternative for everyone.
“You’ve got to be able to identify where in the brain the seizures are coming from and be able to safely remove or ablate that,” he said.
“There are certain parts of the brain where you can operate on and remove quite safely.”
But he said if the target was “really deep in the brain” or near areas that played a key role in critical functions, such as memory or cognition, traditional surgery risked doing more harm than good.
That was the case for Melbourne videographer Cal Croft, 29, whose seizures were triggered by a tumour in a sensitive area of his brain.
He said, when he was younger, a surgeon tried unsuccessfully to remove the tumour.
“It was just too dangerous,” Mr Croft said. He was one of the first patients to undergo LITT at the Alfred and has been seizure-free since the surgery last October.

Mr Croft’s seizures, which had been mostly controlled by medication, suddenly returned in his late 20s.
He said he was unable to drive and the seizures, and his increasingly high doses of medication had a big impact on his life and memory.
“There’s six months or so where there’s parts I just don’t remember,” he said.
By the time he was wheeled in for surgery in October last year, the level of drugs required to stop his seizures was causing side effects including vision problems and tremors.
“It feels like, touch wood, that I’m cured,” he said.

Dr Gutman emphasised that stories like Mr Croft’s and Ms Kenny’s were possible only with a careful, considered program and a huge team of people.
And it’s true – it’s incredible the number of people who, in the space of just a few hours, came together with the sole goal of helping Ms Kenny last week.

They ranged from the anaesthetists and nurses to radiographers and even specialists from the medical device company that makes the laser device, who were in theatre for all operations.
Ms Kenny, speaking just days after her surgery, said she was discharged the next day and everyone involved had been “just absolutely brilliant”.

The 71-year-old woman, who flew in from Adelaide for the procedure, said she had tried dozens of medications and nothing had helped.
“Epilepsy has a total mind of its own,” she said.
“I’ll just have a seizure at any time. It’s horrible.”
A music teacher, Ms Kenny had to give up her licence after crashing her car during an episode, and said the prospect of a seizure-free future was incredible.
“It would be amazing, absolutely amazing, to think I don’t have to have this cloud over my life all the time,” she said.
Originally published as A surgeon, a tiny laser and a cure to blow your mind: Revolutionary epilepsy treatment