Medicine most fears the bugs it can’t stop – now they are here
The case of a Ukrainian soldier whose leg was amputated because British doctors could not treat his infection is a red light that needs global action.

When the soldier arrived from the battlefields of Ukraine, the medical team was – at first – most concerned about his extensive shrapnel wounds. But when they had cleaned up the 35-year-old’s injuries, the doctors at St George’s Hospital in south London realised they had a bigger problem on their hands. Deep within the blast wounds on his left leg, a bacterial infection had taken hold.
An initial cocktail of five different antibiotics failed to kill the bacteria. With the wound still festering, they switched regimens to try four other drugs, including colistin, a “top-shelf” antibiotic with severe side effects that is reserved for cases where nothing else will work. But those, too, had a limited impact.
For decades doctors have warned of a dystopian future in which antibiotics are rendered useless. In that ward in November 2022, the grim prospect was no longer a distant one. In one of world’s most specialised trauma hospitals, surgeons retreated to medieval methods. To save the soldier’s life from the mutated superbugs, they were forced to amputate his leg at the knee.
Luke Moore, an infectious diseases consultant called in to assist on the case, describes antimicrobial resistance, or AMR, a “silent pandemic”. If bacteria continue to evolve to evade drugs it will put even routine healthcare at risk. Removing a child’s tonsils would endanger their life.

Moore says: “Unless we crack this nut, it threatens everything else we do. It threatens our ability to do simple surgical operations; it threatens our ability to provide chemotherapy for patients with cancer.”
World leaders meeting at the UN General Assembly in New York this month will attempt to hammer out an agreement to avert the superbug threat.
Dame Sally Davies, the former chief medical officer for England and now the British special envoy on AMR, says: “We need to move from talking about it to action.”
The St George’s incident was no isolated case. Similar reports have emerged from Norway, The Netherlands and Germany, where hospitals also have provided medical assistance to soldiers evacuated from the Ukrainian frontlines.
Kristian Riesbeck, professor of clinical bacteriology at Lund University in Sweden, conducted a study last year in which he tested samples from 141 patients being treated in Ukrainian hospitals.
“I’ve never seen that kind of resistance,” he says. “It was the worst I have seen. These are very, very resistant bacteria.” In nine samples he tested, the bugs were resistant to every single antibiotic available.

Ukraine is the frontline in the war on superbugs and not only soldiers are affected. Eight of the samples in the study were from newborn babies with pneumonia.
“All patients – soldiers and civilians – end up in hospitals (close to the fighting),” Riesbeck says. “It’s complete chaos and everyone is mixed.”
In such conditions, superbugs thrive. Moore says: “In areas of the world where there is catastrophe and conflict, where they’re being overwhelmed by … people who need help, infection prevention and control is one of the first things to be lost.”
On his way to St George’s the soldier passed through four Ukrainian hospitals: in one he picked up the bug that cost him his leg. “The acquisition of the most difficult to treat bacteria is not next to a ditch on a battlefield, it is almost always in healthcare environments,” Moore says.
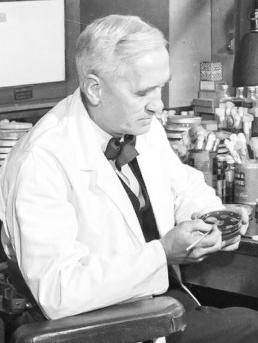
It was Sir Alexander Fleming, whose 1928 discovery of penicillin transformed medicine, who first warned of the fundamental weakness of antibiotics. Accepting the Nobel prize for his discovery in 1945, he said: “There is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant.”

For almost a century antibiotics have been a mainstay of modern medicine. The more they are dished out, the faster germs have evolved to resist them. “Once you start using lots of antibiotics there’s a stronger selective pressure for bacteria to evolve resistance,” says Craig MacLean, professor of evolution and microbiology at Oxford University. The bugs have a trick that helps them evolve – they can swap genes with other strains. “Plasmids are these little circular bits of DNA that can hop around between bacteria and so move resistance genes from one species to another,” MacLean says.
In hospitals, where patients with many infections are concentrated in one place, this is a particular threat, these dancing genetic features swapping between germs. “If there aren’t good infection control procedures in place you get a perfect storm – lots of mixing of bacteria allowing genes to be exchanged and high antibiotic use generating a strong selective pressure for resistance,” MacLean says.
A few decades ago, picking up a resistant bug in hospital was unheard of. These days, with more and more antibiotics being dished out, bacteria are increasingly resistant. In 2014 a British government review projected that resistant superbugs would kill 10 million people a year globally by 2050. But that creeping horror is closer than we thought.
A study in medical journal The Lancet in 2022 found there were 4.95 million deaths in 2019 linked to drug-resistant bacterial infections, of which 1.27 million were directly attributable to superbugs.
An updated Lancet paper with new numbers is due this month. Colin Brown, deputy director on antimicrobial resistance at the UK Health Security Agency, says: “The numbers are only going to go up and up and up. It’s not a problem of the future – it’s a problem of the here and now.”

This is not only a crisis for war zones. In England in 2022 more than 58,000 people acquired an antibiotic-resistant infection, up 4 per cent on the year before. Almost 8000 people die each year in Britain from such infections.
Esme Harris, 92, from Solihull near Birmingham, is vulnerable to lung infections because of a genetic defect called alpha-1 antitrypsin deficiency. Her condition was manageable until she contracted a nasty superbug called pseudomonas. Amoxicillin – the antibiotic she usually used to knock back any infection – stopped working.
“Between March 2020 and November 2022 she was hospitalised nine times by ambulance,” says her daughter, Sue.
Each time she went to the emergency department doctors had to use trial and error, working through antibiotics in turn to see what would work. On one occasion, in April 2022, she almost died because drug after drug had failed. Harris pulled through and doctors put her on a routine antibiotic called azithromycin, which is working for now.
“It’s great that this antibiotic is working and it’s given her such a quality of life,” Sue says. “But at some point that might stop working too. I don’t know at what point the options will run out. That’s true for her and for the whole world.”

Despite the threat, antibiotic prescriptions have risen for three years running, reversing a trend in which prescriptions had been falling since 2014. Last year in England 36.9 million prescriptions were dispensed by GPs and other healthcare staff. Of prescriptions given out by GPs, a fifth are estimated to be for diseases against which the drugs will not work.
Brown says: “We’re doing a trial that is looking at changing wholesale the antibiotics that we give in primary care for urinary tract infections. We want to see if using an alternative antibiotic, with a different resistance protocol, can drive resistance down.”
Davies has been at the forefront of trying to tackle AMR across the globe. A key problem is that GPs may not know whether a sickly child has a virus – for which antibiotics are useless – or a bacterial infection, for which they could be rapidly effective. “This is why we need cheaper, better diagnostics,” she says. Davies will be at the UN meeting later this month.
Without international agreement, reducing the use of existing antibiotics globally is impossible. John-Arne Rottingen, chief executive of the Wellcome Trust, who is also involved in negotiations on the problem, says: “We need to set a global goal, a target of actually reducing the problem and so countries can be held accountable for progress.”
Moore says: “There is no silver bullet ... to win and push back against AMR. But what we can do is slow it down. We need to learn from our mistakes, share that learning and move together internationally. Because this is the next threat to modern healthcare.”
THE SUNDAY TIMES



To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout