One step back, 10 steps forward for stem cells
IT’S full steam ahead at the medical frontier, with regenerative medicine front and centre.
IN case you missed it, 2014 was the year stem-cell research jumped to warp speed. Already a fast-paced discipline, the action began in January when a team of Japanese scientists claimed to have found an almost unbelievably simple way of producing embryonic stem cells. In October, incredible news broke that stem cells from a paraplegic’s nose had enabled him to walk again. And in December it was announced that an extraordinary collaboration involving 50 scientists from around the world — 15 of them Australian — had resulted in a highly detailed road map for how to reprogram cells.
Although one of these breakthroughs foundered, ending in tragedy and disgrace for the scientists involved, the sheer quality and quantity of stem cell research around the world last year made 2014 a game-changer for the field.
First, some background. Stem cells are the wildcards of the genome pack. They are pluripotent, which means capable of generating any type of tissue. As well as replicating carbon copies of themselves, they can differentiate into cells with specialised functions.
The discipline really came into being in the late 1990s, when researchers succeeded in establishing laboratory lines from the inner cells of days-old human embryos. At the time, the possibilities seemed almost limitless. Scientists now had them on tap — generic human building blocks, ticking over in a dish, ready for assignment to any part of the body.
Stem cell therapy loomed as the solution to a multitude of disorders involving tissue damage or loss of cells: catastrophic injuries such as severed spinal cords; late-onset syndromes such as age-related macular degeneration; modern scourges such as Parkinson’s, Alzheimer’s, stroke, diabetes, blood and kidney diseases.
But there was a problem. The source of these wonder cells — four to six-day-old human embryos — presented an ethical minefield. Churches howled in protest. Cabinets debated endlessly. Governments imposed bans. Couples undergoing fertility treatment chose to have their leftover embryos destroyed rather than donate them for research.
Then, in 2006, Japanese doctor and researcher Shinya Yamanaka found a solution. In a study that would win him a Nobel prize six years later, he reprogrammed the skin cells of mice into pluripotent cells functionally very similar to embryonic stem cells. Within a year, several groups had done the same thing with human skin cells.
The world was astonished. These induced pluripotent stem cells bypassed the need for human embryos. And they introduced the possibility of harvesting stem cells from any person with any illness. In theory, researchers could rewind diseased cells to their basal state and study whether some glitch in their original genetic hardwiring had made them go awry.
But there was a problem.
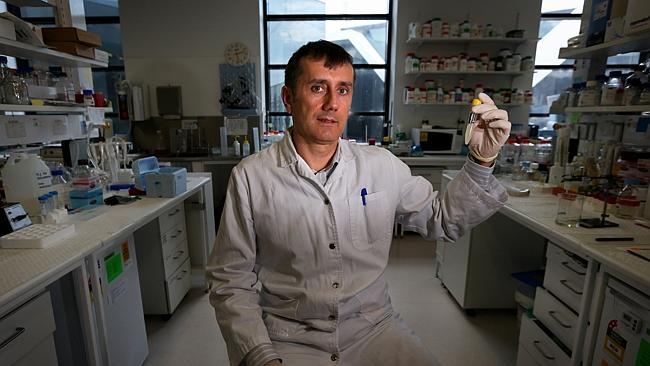
“The initial process of making IPS (induced pluripotent stem cells) was quite deficient,” says Thomas Preiss, a German-born biochemist at the Australian National University in Canberra. “Very few cells actually became reprogrammed.”
Preiss, an expert in the biology of ribonucleic acid — molecules that play an essential role in communicating genetic code — says the Yamanaka technique was “fantastic” as a proof of principle. “But to make it into a usable technology you really have to be able to do this much more efficiently,” he says. Research teams all over the world worked on improving the Yamanaka technique. But then the Japanese-led team hit the ball out of the park in January last year with two papers in the journal Nature. They demonstrated an astonishingly simple way of generating IPS cells by exposing blood cells to mild acid for less than a half-hour.
The world gaped. The so-called “stimulus-triggered acquisition of pluripotency” or STAP technique could quickly and efficiently generate stem cells that were even more malleable than IPS cells. STAP cells could even form placental tissue — something neither IPS cells nor embryonic stem cells could do — offering an easier path to cloning. It seemed too good to be true.
And it was. Alarm bells began ringing as labs around the world failed to replicate the study. Nature launched an investigation and first author Haruko Obokata was found guilty of scientific misconduct. In August, highly respected co-author Yoshiki Sasai committed suicide. Tissue engineer Charles Vacanti, who ran the lab where Obokata had started her work, resigned his chair at a Harvard University teaching hospital. It was a tragic saga and a bad look for stem cell research.
But in the months since, the field has repaired its image as smoothly as researchers believe it will one day repair human tissue. In October it emerged that a Polish and British team had transplanted adult stem cells from a paraplegic firefighter’s nose into his severed spinal cord, enabling him to walk again.
Then, in December, an extraordinary four-year team effort by almost 50 scientists — dubbed “Project Grandiose” — really set the record straight with not two but five papers in Nature and one of its sister journals. The project’s thoroughness, back-to-basics approach, meticulous attention to detail and almost obsessive commitment to disclosure make this study the polar opposite of the Obokata study.
“Probably the biggest difference is that all of the methods and all of the data are very freely available,” says Queensland University stem cell biologist Christine Wells, a senior author of three of the project’s papers. “My role in the project was to make sure the data was acceptable to the generalist rather than the specialist.”
Preiss says the project’s conservative approach should also reassure sceptics, with the team faithful to the Yamanaka technique. “We’re tweaking that process rather than replacing it with something entirely different,” says Preiss, a senior author on four of the papers. “We have described in unprecedented detail the molecular changes that cells undergo as they reprogram into stem cells.”
Overviewing the study in a Nature commentary, Salk Institute geneticists Jun Wu and Juan Carlos Izpisua Belmonte say it provides the first “thorough road map” for cell reprogramming. “In embracing the inherent artificiality of IPSC reprogramming, Project Grandiose has opened up the field to fresh avenues of research.”
The study involved no fewer than 15 Australian researchers with major roles for the ANU, Queensland and Sydney universities, the Victor Chang Cardiac Research Institute and the QIMR Berghofer Medical Research Institute in Brisbane. Preiss says it was a textbook case of global collaboration, with the Australian involvement cultivated during project leader Andras Nagy’s sabbatical in Sydney in 2011.
Preiss says Nagy, a Toronto-based stem cell scientist who holds an adjunct professorship at Monash University’s Australian Regenerative Medicine Institute, had close scientific ties with Australian developmental biologists well before his arrival in Sydney.
“There is a high density of excellent research in genomics, RNA science and stem cell biology around Australia,” Preiss says. “Colleagues elsewhere wouldn’t work with us if we didn’t have something good to offer.”
Project Grandiose achieved more than merely cementing an understanding of how adult cells are reprogrammed to produce stem cells. It discovered an entirely new type of pluripotent cell: the F-class cell, which forms in “fuzzy-looking” colonies, according to Wu and Belmonte.
The discovery means scientists now know of four types of pluripotent cells that can be cultured in the lab: F-class cells, ISC cells, embryonic stem cells and more committed epiblast stem cells. More may be awaiting discovery, Wu and Belmonte say: “Customised stem cells designed for specific applications, such as large-scale expansion or fast, synchronised differentiation, may soon become a reality. The existence of (these) alternative states adds another dimension to the potential of pluripotent stem cells in regenerative medicine.”
With reprogramming back on firmer ground, stem cells derived from adults are looking increasingly promising. And the move from embryonic to induced stem cells is pushing the field from the generic to the specific, with the promise of individually “corrected” tissues rather than universal spare parts.
Wells says this is a game-changer. “It opens up the possibility of treatments where you’re not injecting someone else’s cells, or cells which have been processed in a lab, but your own cells (which have been) trained to do a job that needs doing.”
Wells says this is the future of regenerative medicine, but admits it’s a long-term goal. “We are still so clumsy at understanding why cells are what they are, and how to (extract) different desirable characteristics. It would be a foolish person who jumped straight into a clinic in this regard.”
Preiss says that for most diseases, IPS cell therapies are a decade or two off. But for some they may be just around the corner. Trials of a treatment for age-related macular degeneration are already under way in Japan.
And he says an entirely different type of stem cell research may have immediate applications. “If you create IPS cells from a patient you can differentiate them into a specialised cell type in the laboratory. You have a ‘disease in a dish’ model that you can use to study the disease.
“You can do experiments in a dish that you can’t do on a patient. You can isolate the genetic defect. And you can use cell culture models like that — disease-specific patient-derived cells — for more conventional drug development, for developing new drugs and testing their efficacy.”
Wells says cell reprogramming means all this can be done using skin biopsies rather than taking a chunk of a diseased organ such as a kidney — often impossible. And she says the potential of stem cell research doesn’t end there, with the field promising answers to some of the most fundamental questions of human biology.
“What’s the difference between a blood cell and a heart cell?” she says. “What’s the difference between a scar-forming cell and a smooth skin cell? What’s the switch between a healthy skin cell and a cancer cell? How do you toggle between a function that’s desirable in one context, and undesirable in another?
“It’s an enormously rewarding area because we’re literally unravelling the black box of the human genome . From a philosophy of understanding who we are and how our cells do what they do, we’re getting at the heart of this information process.”
This means the potential of stem cell research isn’t limited to injuries and inherited degenerative diseases. It could yield answers to problems caused by environmental factors such as smoking and diet. “The applications are really only limited by our ability to explore them,” Wells says.
Despite the advantages of ISC cells, many researchers still use stem cells harvested from embryos. Wells says that in some ways they are a purer type of stem cell. “An adult cell that’s been reprogrammed does keep some memory of what it was in its mature form,” she says. “That memory might not be encapsulated in the gene information but it might be in the way that gene information is packaged and available to be used.”
But while ethical objections persist to the harvesting of cells from embryos, she says they have softened with time and a realisation that it’s not about making designer “monster” babies. “Those scary scenarios haven’t played out. Perhaps the general public is more familiar with the concept and less frightened by it.”


