Revealed: sick state of bulk-billing
Doctors predict the bulk-billing rate may plunge to 30 per cent within two years without urgent action.

Doctors expect the national bulk-billing rate may plunge to as little as 30 per cent within two years unless urgent action is taken, as new data from hundreds of the nation’s biggest medical centres casts doubt on the veracity of official Medicare records.
Health Minister Mark Butler says the presentation of Medicare’s figures by governments has sugar-coated the true state of primary healthcare and he has ordered his department to review the “skewed” official data that states 88 per cent of all GP attendances are bulk-billed.
Medical groups label that figure “complete garbage” and have produced their own records that suggest the true bulk-billing rate is closer to 60 per cent and rapidly declining.
People living in some of the most disadvantaged parts of the country are finding it hardest to access bulk-billing clinics amid warnings that universal bulk-billing is in a state of collapse following years of frozen funding.
As local councils in Tasmania step in to take the extraordinary step of funding primary care for residents, Mr Butler said he was particularly concerned at anecdotal reports some pensioners were now being charged gap fees.
“I think if that starts emerging as something other than a sort of black swan event then we’ve got a real issue on our hands,” Mr Butler told The Australian.
He has ordered a tranche of reports from the federal Health Department in order to determine the true national rate of bulk-billing. One issue is the tens of millions of bulk-billed telehealth and vaccination services that have disguised the decline in bulk-billing.
“What we’ve had for the last several years is very much a sugar-coating of what’s happening in primary care, and particularly in general practice, from the government sort of trumpeting these official bulk-billing rates which were skewed,” Mr Butler said.
“And it just doesn’t gel at all with what patients and increasingly doctors are telling us about what’s happening on the ground.
“I’m asking for more and more reports from the department to understand exactly what’s happening. But I’m convinced that things are going the wrong way.”
Latest health department data shows national GP bulk billing rates have declined by 1.5 per cent in the past six months as thousands of doctors reduced bulk billing services. The June quarter 2022 bulk billing rate was 87 per cent.
It comes as the Australasian College for Emergency Medicine warned that emergency departments were “dangerously overloaded” because over a long-term period many people have not be able to access or afford the care they need in the community “Without access to appropriate care, people get sicker, their health deteriorates, and their acute conditions become chronic,” the college said. “Then, when things get unbearable or unmanageable, and they are suffering immensely, they present to EDs for urgently needed help.
“The worst part is, this could all have been prevented by access to affordable, accessible, integrated primary and community-based care over time.”
According to Medicare data just published, the national bulk-billing rate for GP attendances was 88.3 per cent in 2021-22. The Australian can now reveal data from 500 of the nation’s biggest medical centres that casts doubt on the official bulk-billing rate.
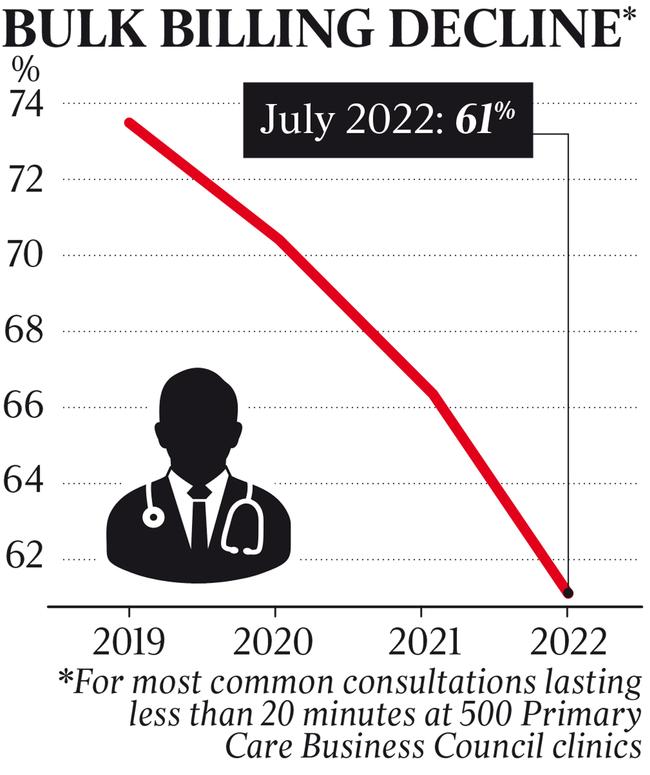
The Primary Care Business Council has compiled statistics analysing all cases of the most common type of GP visit – a 20-minute Medicare Benefits Schedule Item 23 consultation – and calculated the percentage of those consults that were bulk-billed. The PCBC represents the seven biggest corporate operators of 500 GP clinics nationally.
The statistics reveal that the rate of Item 23 consults that are bulk-billed has dropped to an average of 61 per cent across the 500 clinics, a 12 per cent decline from two years ago. The rate for one of the operators is just 36 per cent.
Jeremy Stones, CEO of corporate operator Better Medical, said the official Medicare data was “misleading”.
“The official data that would imply that for every 8.8 visits out of 10, there is no out-of-pocket cost, which is manifestly not right,” he said. “If you really want to look at the underlying trend of Australians paying increasing out-of-pocket costs, you look at the trend of Item 23, which is the most common MBS item. And on that trend, it’s approaching 60 per cent within the PCBC network. I would estimate it will continue to decline into the low 40s or high 30s by the end of this year.”
Doctors say one of the reasons Medicare statistics are inflated is that in many privately billed consultations, a patient presents with multiple issues, so the GP attaches a co-payment to one of the MBS item numbers and then bulk-bills for the other item numbers. “Most doctors will just charge a single gap but then bill both items which then gives government the impression that that patient is being bulk-billed when they’re not,” says the president of the Australian Society of General Practice, Chris Irwin.
Enormous numbers of GP clinics have begun writing to their patients in the past weeks advising they would no longer bulk-bill, prompting doctors’ groups to warn universal bulk-billing is on the brink of collapse.
The crisis is acute in Tasmania, where very few practices bulk-bill all patients despite the state having lower than average incomes.
In Huonville, southwest of Hobart, the Huon Doctors Surgery, which was 100 per cent bulk-billing, now charges all patients a gap fee. That includes 79-year-old pensioner Darrel Doyle, who is charged a discounted $60 per consultation. Mr Doyle gets $39.75 back from Medicare, leaving him with an out-of-pocket cost of $20.25.
“It certainly makes things harder with the cost of everything else going up,” Mr Doyle said.
Huon Doctors GP Jason Lemon said doctors felt sad about having to charge pensioners.
“We didn’t want to have to do it,” Dr Lemon said. “Our patients are from a rural area, they’re disadvantaged, they don’t have 2 two cents to scrape together.
“They’re putting their health issues on the backburner because they can’t afford to come in and have them dealt with. We’re sending at least one person a day off to hospital via ambulance because they’re presenting either so unwell or with serious health conditions that are too complex for us to deal with in general practice.”
Tasmanian Premier Jeremy Rockliff is calling on the Albanese government to urgently boost incentives for GPs to work in regional areas, as the state and even cash-strapped local councils step-in to fund rural doctors.
Mr Rockcliff is pushing a “bold” pilot plan that would see states pay GPs a salary to work in state rural health facilities, and the state is also funding GPs and pharmacies to offer after-hours services. Mr Rockcliff told The Australian federal Labor needed to “step up” by funding the scheme – and improving its own incentives.
“While the Tasmanian government is doing all it can to assist general practice with innovative solutions, the federal government needs to come to the table – and provide additional supports and incentives, to ensure the long term sustainability of GP practices,” he said.
The Glamorgan Spring Bay Council, in the state’s east, has started using ratepayer levies to supplement the costs of running local GP services and lure doctors. In Glamorgan Spring Bay, which has a higher than average proportion of elderly residents, the 5200 ratepayers pay a $90 levy to help fund private and council-run GP services. Mayor Robert Young said the council used the levy, and some general revenue, to plough up to $600,000 each year into funding local GPs.
“We need doctors and it’s very difficult to get them to come, so we do what’s necessary to get them,” Mr Young said. “Our people are old. We’re like used cars. If we don’t get regular repair and maintenance, we’ll stop going.”
Dr Irwin said doctors were extremely concerned about access to primary care among vulnerable regional patients. He estimates the true national bulk-billing rate – which has been inflated to some extent by mass bulk-billing of telehealth and vaccination consults during the pandemic – is probably close to 60 per cent.
“I think that may fall to about 30 per cent or so over the next year or two if the government doesn’t take urgent action,” he says.
“The government has been using these misleading statistics for a while to try to sort of push the agenda that all is well and that they can freeze Medicare for a decade and have no adverse impact on patients. But it’s completely wrong. The bulk-billing statistics are complete garbage,”
The Medicare rebate for many general medical services items increased by 1.6 per cent in August but the rebate has been frozen for six of the past nine years.
How to address the crisis in general practice is being examined by the Strengthening Medicare Taskforce that Mr Butler chairs as the government plans how to spend $750m is has earmarked for general practice. It will report by the end of the year.






To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout