Rebate freezes have ripped $3.8bn out of Medicare
The erosion of the Medicare rebate is hitting the most vulnerable hardest, with new analysis revealing almost $4bn was denied to patients in rebates | CHECK YOUR REGION

The erosion of the Medicare rebate is hitting the most vulnerable Australians hardest, with new analysis revealing almost $4bn was denied to patients in rebates under years of freezes.
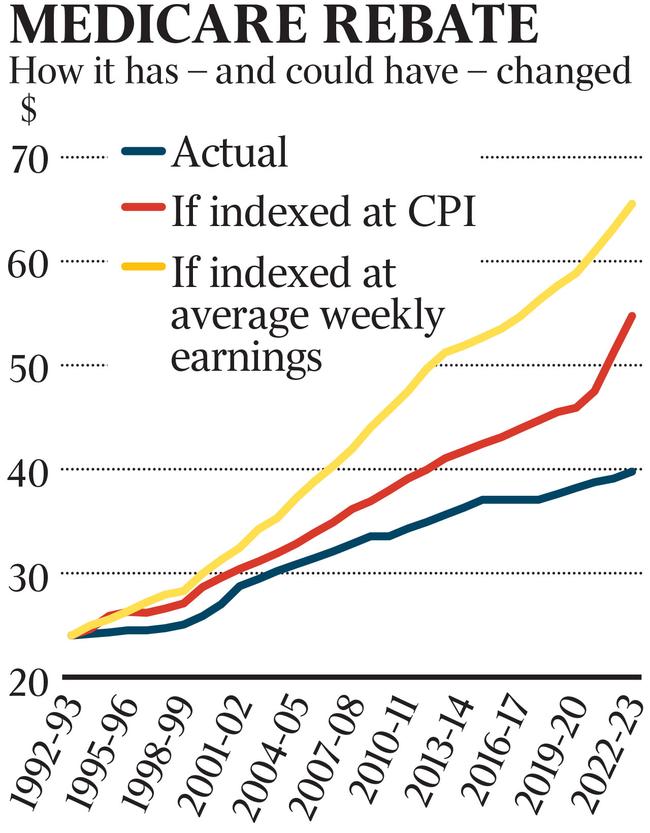
That comes on top of decades of paltry indexation that has led healthcare subsidisation to fall behind the cost of living.
Federal Health Minister Mark Butler has said “nothing is off the table” in this year’s budget but is refusing to show his hand on whether the government will move to increase rebates as pressure grows to take decisive action, with the general practice sector failing to meet patients’ needs for access to doctors and affordable healthcare.
Doctors blame grossly inadequate rebates for the crisis gripping the sector, with new analysis by the Australian Medical Association for the first time quantifying the amount of money – $3.8bn – “ripped out of Medicare” in years of cost-cutting that has contributed to plummeting rates of bulk-billing and unfeasible wait times for appointments.
If the indexation rate is not lifted, the flow-on effect of the years of frozen indexation is predicted to amount to more than $8bn by 2028 – an amount the doctors’ lobby says is based on “very conservative assumptions”.
AMA president Steve Robson said low patient rebates were a key reason that bulk-billing rates had plunged to their lowest level in a decade. Patients are waiting longer than ever to access a GP, and the primary care system as a whole is struggling to survive.

“The most vulnerable people, the people with chronic conditions, the ones who have to see a GP the most, are paying the biggest penalty,” Dr Robson said. “And when they can’t find a bulk-billing GP anymore, the only option is public hospitals. And we’re seeing a catastrophe within our public hospital system.”
The AMA is demanding all of the money the commonwealth government has saved from freezing Medicare indexation now be returned in the form of an immediate lift to the Medicare rebate, which for a standard consultation currently sits at $39.75. Many patients are charged a gap fee of $40 or more. The rebate increased by only 65c between 2020-21 and 2021-22.
The Medicare indexation rate has averaged 1.1 per cent for the past three decades, while CPI and Average Weekly Earnings have risen on average 2.42 and 3.53 per cent respectively in the same period. Inflation is eroding the rebate in real terms even further.
“You need a microscope to see the increase in funds each year, it’s just crazy,” Professor Robson said. “It’s less than a dollar increase in an environment where inflation has been approaching 10 per cent in some areas. A lot of practices have just reached the point where they really can’t absorb this anymore.”
Government figures show fewer than two-thirds of patients nationally are always bulk-billed, and just over 20 per cent are usually bulk-billed. Regional health patients have some of the lowest bulk-billing rates in the country, notably in Tasmania, where only 45 per cent of patients are always bulk-billed, northern Queensland with 58 per cent, and country SA and WA where only half of patients are always bulk-billed.
“As a country, we need to ask ourselves what is Medicare all about?” Professor Robson said. “Is it about ensuring care for the people who most need it is affordable? I think we’re seeing at the moment the wheels are really falling off the cart in affordable care and access to care for Australians who most need it. That’s a huge concern not only for doctors but society as a whole.
“We’re at a point now where we’re going to have to do something.”
The federal government has committed $750m over three years to strengthening Medicare and plans to implement reforms recommended by a recent taskforce report in this year’s budget, including opening up funding to nurses and allied health.

Mr Butler recently told a pharmacy conference the government needed to find “hundreds of millions of dollars” in the health budget to fund core programs in digital health, dental and after-hours GP services that he claimed had not been funded in the forward estimates by the previous government. He would not be drawn on whether the government would move to lift the Medicare rebate as well as implement structural reforms to Medicare despite promising that “there is no higher priority in health for the Albanese government than rebuilding general practice”.
“Strengthening Medicare after a decade of cuts from the former government will take more than one budget but we are determined to get this right,” Mr Butler said.
The AMA released its analysis of the rebate erosion along with the GP chapter of its 2023–24 budget submission which calls for investment in general practice beyond the $1bn the government committed to in the last election.
It wants the government to fund the delivery of GP care in aged care facilities, provide greater support for chronic wound care that will save more than $200m over four years from reduced hospitalisations, and also provide funding for team-based care and longer GP consultations.
More Coverage







