Overrun hospitals not prepared for Covid-19 crisis
The health system is so overburdened by Covid-19 that people are dying from other conditions as patients are stuck in ambulances, corridors.

Doctors have warned that the health system is so overburdened by Covid-19 that people are dying from other treatable conditions as patients are stuck in ambulances and the corridors of emergency departments, unable to access a hospital bed.
A discussion paper drawn up by top health officials from four states and presented to a recent urgent roundtable of health ministers warned the hospital system was buckling under the strain of not only Covid-19 but also routine care, while doctors warned conditions deemed low priority would develop into life-threatening emergencies as treatment was deferred.
The health officials said the government should consider deploying GPs to hospital emergency departments to tackle workforce shortages.
Thousands of patients should be transferred home for treatment to take pressure off hospitals, and the government should embark on an urgent immigration program to boost doctor numbers.
It also called for the federal government to fund GPs to operate after hours and on weekends to address the indirect impacts of Covid-19 on the hospital system.
In addition to Covid-19, hospitals were also facing pressure from rising emergency department presentations, ambulance access block, workforce burnout and the diversion of frontline staff to testing and vaccination centres.
The pressures on the system have been exacerbated further by a critical lack of support in the community for elderly and disabled patients who cannot be discharged and are spending sometimes as long as a year in hospital, taking up beds.

National cabinet on Friday will be presented with a plan for surge ICU capacity as the hospital system comes under attack from rising case numbers as NSW and Victoria prepare to lift restrictions.
The Australian Medical Association backed the warnings, saying patients were facing a “perfect storm” as ward space continued to shrink as more people were hospitalised with Covid-19.
“The health system doesn’t look after just Covid and it’s already full,” said AMA deputy president Chris Moy. “We’re seeing that Covid on top of the existing chronic pressures is a perfect storm and it is really basically causing the hospital system it to overflow and be overwhelmed.
“What happens is people either don’t get care or it gets displaced. Diagnoses are made at much later points, and people get worse or they die. Adverse outcomes will be increasingly likely.”
Scott Morrison is facing calls to boost funding for public hospitals as Friday’s national cabinet meeting discusses the ICU surge plan to cope with higher case numbers as states open up.
NSW Health Minister Brad Hazzard said much more than an ICU surge plan was required to make sure hospitals did not collapse as case numbers rise.
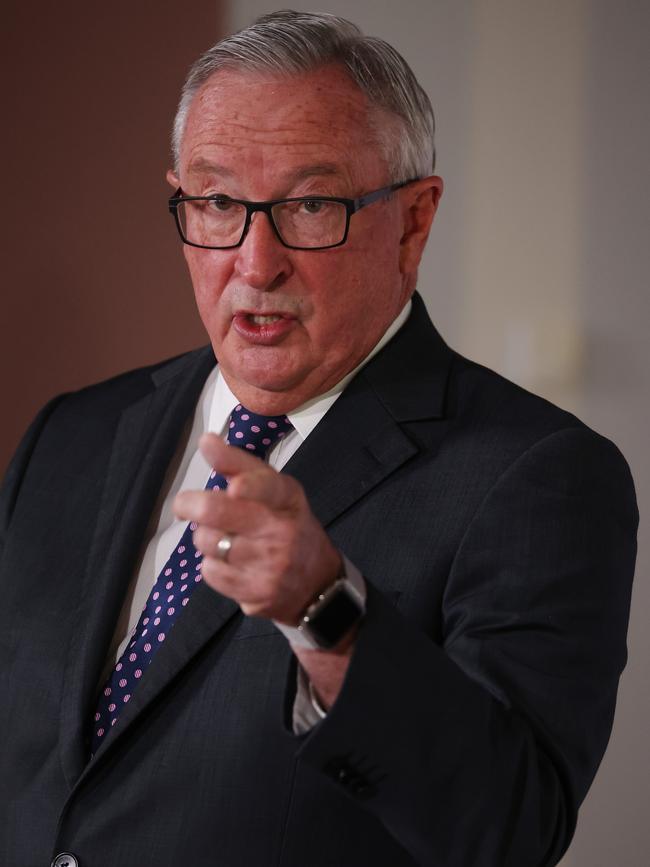
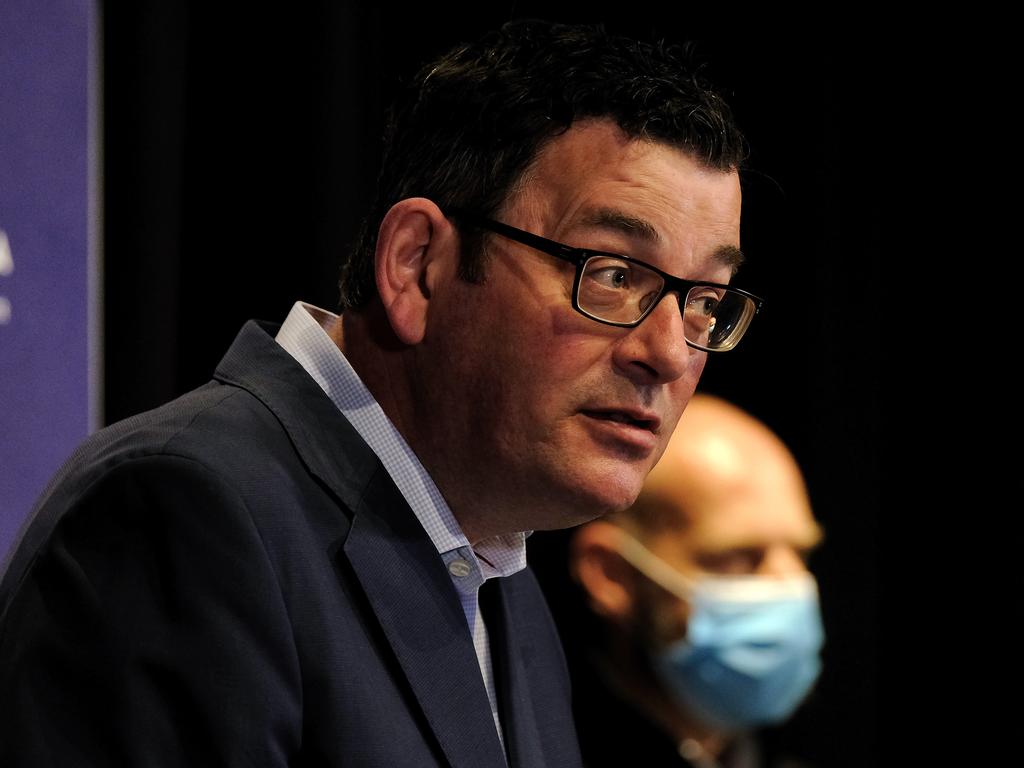
“It’s far too narrow, it doesn’t meet the growing need. It’s a stopgap,” Mr Hazzard said. “Every state and territory minister is concerned about the increasing demand on our hospital system and have expressed the need to the federal government for an increased and changed funding model.” Victorian Health Minister Martin Foley said it was not clear that hospitals would be able to cope with the rise in cases predicted under the national road map for reopening as day-to-day patient care was displaced by the pressures of Covid-19.
“The past 20 months have seen all of the existing problems in our health care and in our hospital system amplified to the level where the system is in crisis like it’s never been, in every state,” Mr Foley said. “Now the hour has arrived where without urgent and immediate support from all levels of government, our ability to keep our public health system intact in order for the states to deliver the national plan for reopening with functioning hospitals is at risk.”
The Australian College of Emergency Medicine said the numbers of patients waiting many hours or even two days in emergency departments was increasing, and doctors were struggling to admit even urgent heart attack patients to wards as beds were co-opted for Covid-19 patients.
“In general right across Australia acute patients are waiting unreasonable amounts of time in emergency departments because the hospitals are full, the system is cumbersome and it’s made worse by Covid,” said ACEM president John Bonning. “Patients are being treated in corridors. People with pneumonia, complications of diabetes, patients with strokes, patients with heart attacks, patients with trauma are sometimes struggling to get a bed for as long as 24 hours. It is dangerous.
“The safe nursing ratios have gone out the window. And I would suggest it’s highly likely that patients missing out on elective procedures could result in deaths.”
The performance of non-urgent elective surgery is currently suspended in NSW and Victoria, with the suspensions likely to be ongoing for months.
Sydney urological surgeon Henry Woo said he feared that could result in adverse outcomes and deaths. “There are a number of cancers which aren’t considered to be urgent but they are essential procedures and by kicking the can down the road, it does run a risk that in a number of these situations, the delay is going to lead to inferior outcomes,” said Professor Woo, who is a surgeon at the Chris O’Brien Lifehouse cancer centre and a professor of urology at the Australian National University. The discussion paper warned the challenges to the hospital system were unprecedented but as more people are treated in hospital in the home, GPs could not manage as they were not funded to do so.
“The pandemic has presented challenges to our system and our workforce that we have never seen before,” the paper said.
“Our health workforce pivoted swiftly to respond to the pandemic, working longer, harder and in more challenging conditions than ever before. Patients have also felt significant impacts, particularly those who have experienced deferred care.”
Shocking examples of deferred care leading to adverse outcomes were documented in the discussion paper, including a patient who was unable to obtain podiatry care during lockdown in Victoria and whose routine condition progressed to a critical stage leading to a toe amputation.
There were also documented examples of nurses struggling to cope with the demands of Covid-19 leading to increases in sick leave and resignations.
“We are exhausted. Last night was brutal,” was the testimony of one nurse. “We literally hit capacity, we’re just holding on. None of us have ever faced anything like it.”
A spokesman for Federal health Minister Greg Hunt said that the Coalition had increased total funding to state hospitals by 71 per cent since 2013.
“All ministers recently signed onto a five-year agreement which includes an additional $35bn in funding,” Mr Hunt’s office said. “We’ve also invested an additional $6bn in hospitals funding through the Covid-19 pandemic.
“Commonwealth funding for hospitals increases from $26bn, to $27bn, to $29bn to $30bn per annum, having been $13bn when we came into office. There is no barrier to any state or territory matching or exceeding the commonwealth investment in their own hospital systems.”
Last year the federal government provided a funding guarantee to states and territories that no jurisdiction would be left worse off as a result of the rising costs on the healthcare system caused by the Covid-19 pandemic, but the guarantee expired earlier this year. A national partnership agreement is in place to provide financial assistance to states for the additional costs incurred by responding to Covid-19, but the states are pushing for the Commonwealth to fund half of all costs, up from 45 per cent.







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout