More money than ever but hospital queues keep growing
One third of urgent cases failed to receive on-time treatment in the nation’s emergency departments.

One third of urgent cases failed to receive on-time treatment in the nation’s emergency departments and patients are waiting longer for elective surgery even as governments pour more money into the health system, the Productivity Commission has found.
The commission’s annual report into government services finds the performance of the nation’s hospitals is declining, with Victoria, South Australia and Tasmania experiencing the sharpest drops.
The report shows one in four patients deemed to be experiencing an emergency health condition were not treated within recommended timeframes, while only 67 per cent of urgent cases were seen on time.
Doctors and nurses working in emergency departments say they are often unable to treat the sickest patients in a timely manner because they’re busy caring for patients who need to be admitted to hospital but can’t access a bed.
“Long stays in emergency departments of the most sick and injured are getting longer and longer and are in some jurisdictions really unreasonable,” said Australasian College for Emergency Medicine president John Bonning.
“Some patients are waiting more than 24 hours in emergency departments. Those people require admission but they can’t get a bed. They’re the sickest patients and they’re waiting enormous amounts of time in some cases for a bed.”
The report shows that the performance of emergency departments in treating non-urgent cases improved nationally in 2019-20, with 93 per cent of patients treated on time. For semi-urgent cases, 76 per cent were treated on time, a slight improvement compared with five years ago.
Performance of emergency departments in Victoria has declined markedly over the past decade. Ten years ago, 83 per cent of patients experiencing a health emergency were treated within target time frames in Victoria, while that figure now stands at 67 per cent.
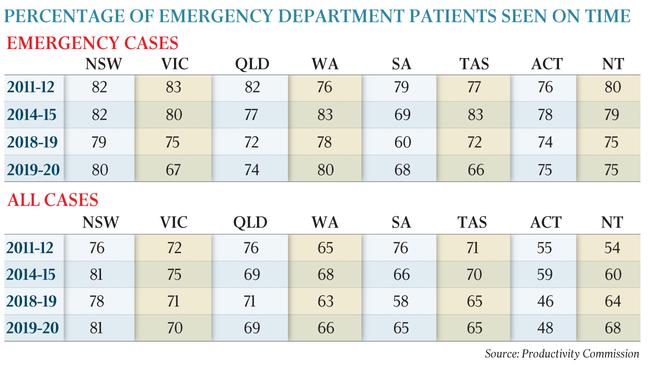
The number of emergency patients treated on time in South Australia has also fallen over 10 years from 79 per cent to 68 per cent.
In Tasmania, 77 per cent of emergency patients who present to hospital were treated on time 10 years ago, while only 66 per cent were seen within target time frames in 2019-20.
The performance of emergency departments across all patient triage categories improved over the past 10 years in the Northern Territory.
The report shows that total recurrent spending on public hospitals reached a record level of $72.2bn in 2018-19.
Government recurrent spending on public hospitals was equivalent to $2851 in 2018-19, up from $2787 per person in 2017-18. Dr Bonning said despite the rising expenditure by governments on hospitals, the increased funding had not kept pace with population growth and the increasing prevenance and complexity of chronic health conditions.
There was still too few hospital beds for those who need them, he said.
“Patients continue to pour in the front door of emergency departments but we’re stuck with all these patients who need to be admitted, who require longitudinal care,” he said. “A third of our workload currently is spent looking after admitted patients that should be on the ward getting their care.
“We need more resources across the system for this relatively predictable number of patients.
Because at the moment the lack of resourcing is manifest in the emergency department where we end up carrying the risk, carrying the can.”

Within hospitals generally, the number of “sentinel events” in which people died or were seriously injured as a result of hospital system error or process deficiencies has declined in the past few years. Nationally, there were 66 sentinel events in 2018-19, down from 81 in 2017-18 and 95 the year prior to that.
As well as access block in emergency departments, the PC report also shows that people are waiting longer for elective surgery, with COVID-19 surgery suspensions particularly placing pressure on Victoria’s waiting lists.
Nationally in 2019-20, 837,839 people were added to public hospital elective surgery waiting lists, while only 688,302 were operated on. The percentage of patients who are cleared from waiting lists annually in 2019-20 was 82 per cent, compared with 88 per cent in 2013-14.
In Victoria in 2019-20, more than a quarter of people had faced “extended waits” on elective surgery lists, up from 12 per cent the year before. Almost half of those that fell in the second-highest clinical urgency category had been waiting more than 90 days for surgery in Victoria. That figure was 16 per cent in NSW.
In Tasmania, elective surgery waiting lists are in a dire state, with more than half of patients across all categories of urgency facing extended waits.
Australian Healthcare & Hospitals Association chief executive Alison Verhoeven said elective surgery waitlist statistics would continue to worsen as the full impact of the COVID-19 surgery shutdown became clear, but that the problem was deeper than the pressure put on hospitals by the pandemic.
“Waiting times for elective surgery in public hospitals will continue to be problematic while we under-invest in both primary care and in public hospitals,” Ms Verhoeven said.
“It’s not acceptable that patients in some states and territories have very long waits for surgery, and national effort is required to change this.
“But we also need to ensure that people have good access to primary care services to assist in reducing the numbers of people who end up needing surgery.”
“One of the things that’s happened over the last seven to eight years has been the freeze on the Medicare rebate, and the closing down of after-hours GP services. When it’s more difficult for people to see GPs at an affordable price then we see people get sicker and then we see more people needing elective surgery.”
Jennifer Doggett, chair of the Australian Healthcare Reform Alliance, said people were waiting too long for elective surgery in almost every state and Territory. “I think it highlights that the capacity in the public hospital system really does need to be beefed up. I think putting more resources into elective surgery and into public hospitals is long overdue and needs to be done.”








To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout