Frontline’s dual strains of worry: sick healthcare workers and rising hospital admissions
Doctors fear infections in health workers and rising hospital admissions could seriously undermine the system.

Senior doctors are growing increasingly concerned that the double whammy of coronavirus infections in healthcare workers and rising COVID-19 hospital admissions could seriously undermine the health system’s capacity to cope.
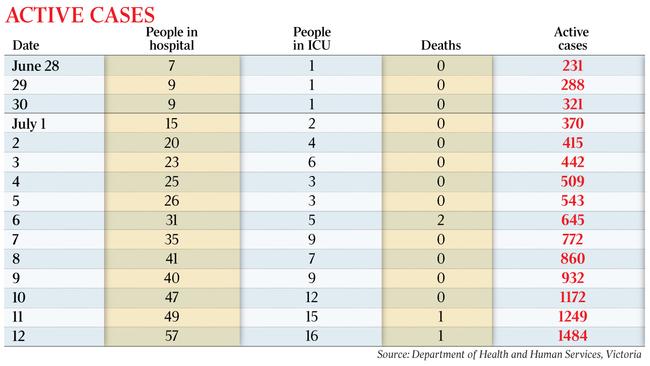
A fortnight ago, when Victoria had 231 known active cases of coronavirus, there were just seven COVID-19 patients in the state’s hospitals, only one of whom was in ICU.
Those numbers have steadily risen in the intervening 14 days, to 1484 known active cases on Sunday, with 57 people in hospital, 16 of whom were in intensive care.
Four people, including men in their 60s and 70s, have died in that time.
The numbers show a 540 per cent increase in active cases, a more than 700 per cent increase in hospital admissions, and a 1500 per cent increase in ICU admissions. Compounding the problem is the potential for healthcare workers to catch the virus, as highlighted over the weekend by new cases in a cluster of at least eight at The Alfred, Melbourne’s key trauma hospital, as well as in an outbreak of 11 cases linked to Brunswick Private Hospital in the inner north.
This month alone, there have been infections in workers at nine other Melbourne hospitals, including the Royal Melbourne and St Vincent’s, as well as a cluster of 11 linked to nine staff at the Northern Hospital’s emergency department.
Hundreds of co-workers have been forced into quarantine and unable to work as a consequence.
As another 273 COVID-19 cases were added to Victoria’s tally on Sunday — the second-highest daily number since Friday’s record 288 — Chief Health Officer Brett Sutton warned the state was facing “the public health challenge of our lifetime”.
“We haven’t even gotten to a peak with this epidemic. We have to throw absolutely everything at it,” he said.
While Victoria invested $1.3bn in early April to boost its 476 ICU bed capacity by 4000, those beds are no use if those who staff them are ill or in quarantine.
The state has more than 1000 ventilators, with several thousand more on order.
“It‘s still a challenge to have a lot of additional cases in ICU,” Professor Sutton said.
“A lot of emergency departments run pretty tight under normal circumstances.
“The number of hospitalised in terms of overall bed capacity … is relatively small, but it becomes challenging when there are hundreds of healthcare workers who are furloughed, who have been close contacts and have to be identified and do 14 days in quarantine.
“That’s an additional strain, but I know that all the hospitals are responding to that appropriately.”
Professor Sutton said healthcare workers were “the last line of defence” against coronavirus.
“My thoughts go to those frontline workers,” he said.
“I‘ve been an emergency department doctor for years, and they are brave and they are brilliant in responding to the challenges of positive cases.”
Professor Sutton worked as an emergency physician in the UK and Australia for more than a decade, including as deputy and acting director of the northwest Tasmanian emergency department.
Asked when he expected the current wave of infections to peak and how big it might be, Professor Sutton said he did not know what to expect.
“We have to reinforce that it is in everyone’s hands, so there is no magic forecast that I can give because I don‘t know if everyone is going to do the right thing,” he said.
Victorian Premier Daniel Andrews said that while healthcare workers were the “last line of defence” in the battle against coronavirus, it was ordinary Victorians who were on the front line.
“If every one of those (on the) front line do the right thing, then we will get past this,” he said.
“The opposite is true, of course. If we don‘t follow the rules, if we don’t play our part, then we will simply see this virus continue to spread, and it will be a longer second wave, a more pronounced, a more tragic second wave than it ought be.”
Western Health’s infectious diseases head Marion Kainer said she was concerned about the recent increase in hospitalisations and the potential for the health system to become overwhelmed.
Dr Kainer said hospital admissions did not tend to occur until day six or seven after a patient had become infected, and ICU admissions several days after that, so numbers would continue to rise even after a flattening of the curve was evidenced.
“I’m expecting hospitals are going to continue to increase patient admissions, including in ICU, over the next few weeks — we have not seen the peak of this,” she said.
“At Sunshine (hospital) we are watching this very carefully. We haven’t had to enact our surge plan and we really hope we don’t have to … because we know the care is better for our patients.”
Dr Kainer said Australia had so far been the envy of the world, given our relatively low mortality rates — about 22 per cent for a patient who required ventilation compared to 60 per cent in some overseas jurisdictions.
She said a major contributing factor was that local hospitals had so far avoided becoming overwhelmed by rising admissions.
“Our first preference is obviously not to have to admit people to ICU,” Dr Kainer said.
“But when we do we want a slow, steady stream so … we can provide the best possible care.
“If they all get slammed, of course hospital staff will always do their utmost, but it‘s not feasible to give patients that dedicated, finetuned care.”

She said prevention had to play a significant role in the public health response.
“It’s so, so critically important that the general population step up and do their civic duty and protect our health system.
“We like to talk about heroes a lot but not everyone will have the opportunity to save someone’s life from drowning.
“But here is an opportunity for every person in Melbourne to save, not just a life, but many lives.
“Those tiny, little decisions each person makes can have a profound impact.”
For Sunshine Hospital emergency department doctor Nish, who asked that his surname not be published, the possibility of contracting the virus is never far from his mind. He’s been wearing a face mask whenever he leaves his home and has been tested for coronavirus four times; the latest being last week after two colleagues tested positive.
“It’s scary with the (case) numbers going as high as they have been and now we are seeing presentations of people who are known to be COVID-positive every day,“ he said.
“We risk our own health and it’s part of our job … but it’s stressful. We just want everyone to do the right thing.”







To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout