Coronavirus Australia: COVID-19 blunders that cost lives
Health Department blunders in two states led to major outbreaks, including two clusters responsible for more than a third of Australian deaths.

Health Department blunders in two states have led to major coronavirus outbreaks, including the nation’s two most deadly clusters which are responsible for more than a third of the Australian deaths from the pandemic.
At the heart of the Newmarch House crisis is lax infection control that has contributed to a death toll that on Tuesday reached 16, the nation’s second-deadliest outbreak.
The Australian can also reveal that Victoria’s largest outbreak of COVID-19 was given a three-week headstart, after the state’s Health Department decided a Melbourne abattoir was not considered an “exposure site” because an infected worker had not been at work while infectious.
The Department of Health and Human Services said on Tuesday night that the first case of COVID-19 linked to Cedar Meats was diagnosed on April 2, three weeks before a second case was identified as part of a cluster that has now reached 45 infections.

As calls grew for an inquiry into Newmarch House, it emerged a contractor at the home was stood down on Tuesday for allegedly breaching infection-control measures at the facility. The Australian can reveal that personal protective equipment was also found dumped in a neighbour’s yard, raising further questions about its infection-control regimen.
Together with the 19 people who died after being aboard the Ruby Princess, in the nation’s most deadly COVID-19 cluster, a total of 35 deaths have come from the cruise ship and Newmarch House residents, a third of Tuesday night’s national total of 97 fatalities.
The special commission of inquiry into the Ruby Princess was told on Tuesday that NSW Health protocols were not followed prior to it docking in Sydney on March 19, sparking a cluster that produced more than 700 COVID-19 infections across the nation, as well as cases in New Zealand and North America.
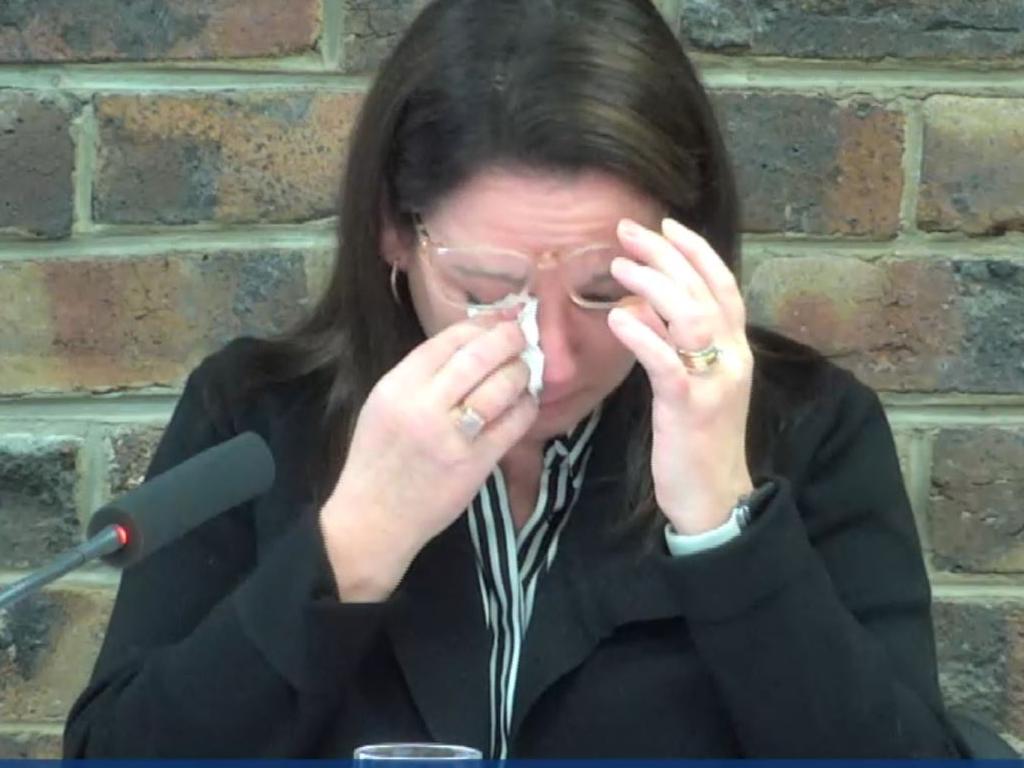
Kelly-Anne Ressler, a senior epidemiologist with the NSW Health public health unit, tearfully told the inquiry that the crucial public safety protocols were not followed. She also revealed that a laboratory oversight delayed infection-control efforts by almost 36 hours. She conceded COVID-19 testing on 15 passengers was accidentally delayed because samples were not flagged as a priority by the government’s laboratory.
The delay resulted in passengers being informed of their health and contagion risks a day and a half after they disembarked from the ship to board shuttle buses, taxis, trains and flights home.
The crisis at Newmarch deepened on Tuesday, with three more staff testing positive to coronavirus. The facility has begun daily testing of staff for the virus after growing pressure from family members to improve infection control. A contractor employed by Aspen Medical, a private provider brought in to boost services at Newmarch House, was stood down by operator Anglicare for the alleged breaches.
There are now 66 infections linked to the nursing home — 29 staff and 37 residents — since the outbreak emerged on April 11 after a part-time carer worked six shifts while exhibiting “minor symptoms”.
A spokesman for federal Aged Care Minister Richard Colbeck said: “The circumstances at Newmarch are being reviewed by the Aged Care Quality and Safety Commission and the public health unit of the Nepean Blue Mountains Local Health District.”
Federal Labor’s aged-care spokeswoman, Julie Collins, urged the aged-care royal commission to lead the investigation into “what went wrong” at Newmarch House.
The federal government stepped in to provide “unlimited workforce support” two weeks ago in what many described as a federal takeover.
Anglicare scrambled on Tuesday to block the facility near Penrith from the public’s view after neighbours accused it of “dumping” medical waste on a nearby property following the discovery of personal protective equipment tangled in a resident’s front bush last week.
Martin Kuppan, who has lived next door to Newmarch House for 15 years, said it took Anglicare two days to clear discarded personal protective equipment from his frontyard.
Appearing before the Ruby Princess inquiry, Ms Ressler was reduced to tears under questioning from commissioner Bret Walker SC, who branded a series of NSW Health shortcomings “reprehensible” and “unsatisfactory”.
“Commissioner, all I can say is that I’m very sorry it turned out the way it did; it was not our intention,” Ms Ressler said. “Myself and my colleagues at the public health unit were working very hard on this. We did what we could, and if we could do it again it would be very different.”

The Ruby Princess was graded “low risk” by a NSW Health expert panel. The decision to allow the ship to dock and its 2700 passengers to disembark created the nation’s biggest coronavirus spike. More than 700 cases of COVID-19 nationally have been traced back to the ship, including a substantial secondary cluster in northwestern Tasmania that shut down two hospitals.
The decision to grade the ship “low risk” came after it provided outdated patient logs to NSW Health authorities. The Australian revealed last week that, had updated logs been provided to NSW Health, the ship would likely have been given a “medium risk” rating, which would have triggered health screening measures.
Mr Walker became frustrated as he questioned Ms Ressler about national protocols for managing the coronavirus on-board cruise ships. They were introduced by the federal and NSW governments as the COVID-19 pandemic escalated. Ms Ressler agreed that lax adherence had been “unsatisfactory”.
NSW Health appeared to acquiesce to cruise ship companies, which tended to apply their own protocols for determining which passengers should go into self-isolation.
Ms Ressler said the companies were resistant to the more stringent levels enforced by NSW because it would mean isolating passengers with minor coughs and colds, potentially ruining their holidays.
Mr Walker branded Ms Ressler’s characterisation of “little old NSW and great big cruise ships” as both “unrealistic and offensive”.






To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout