Coronavirus: Living in testing times
The next stage in managing COVID-19 is identifying the profile and location of risk groups in our community.

The next stage in managing the COVID-19 pandemic here and overseas is identifying the profile and location of risk groups in our community who could trigger the anticipated deadly second wave.
By doing that, those among us who are not at risk can get back to work, without having to worry about getting fined for chewing on a kebab, teaching the kids to drive or buying a pot plant from Bunnings.
Any government that thinks voters are going to put up with this sort of enforcement overreach in the longer term needs to get out more. Literally.
We know from our early profiling that our first wave of casualties and carriers was dominated by our inner-urban wealthy elites, regular visitors to western Europe and the ski fields of Japan and the US, along with highly mobile 20-something students living in higher-density urban areas, and backpackers.
This week we turn our attention to data on the likely future sources of community transmission and our feared second COVID-19 wave, starting with those current cases with no known source of infection.
Using the limited data available from NSW, the one state to release this data spatially, we found the demographic groups dominating areas with the highest per capita unknown sources of COVID-19 infection tended to live and work under the radar — on the mobile fringes of mainstream urban society or in farming communities that are currently experiencing low rates of infection.
The rural group includes farm managers, with their seasonal or full-time agricultural workers, walking to and from work and living in cheap rental accommodation on the farm.
The urban group overlaps the first a little and includes casual workers, riding a motorbike to work and living in high-turnover rental homes off the census radar in 2016.
Anything resembling high-density food preparation by a few and delivery to many would be a prime candidate, just like on the cruise ships.
News of a super spreader living in Victoria, causing four cluster outbreaks while working in hospitality, is consistent with this profile.
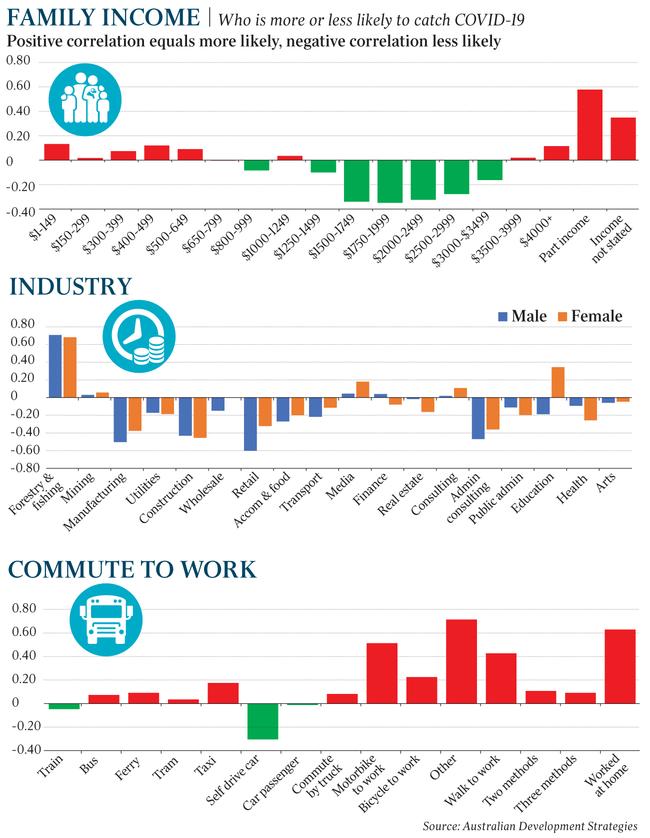
Female teachers are also showing up here. As are small businesses — often one self-employed person living in a family with a partner who is a salary earner. Typically, these are tradies with an irregular income, married to a partner with a (pre-COVID) steady income. These groups are highly motivated to turn up for work whether they’re symptomatic or not, and should be a priority target for point-of-contact antibody testing in future.
The homeless shouldn’t be forgotten either. We should get them off the streets and into temporary accommodation. Both for their protection and ours.
Mainstream suburban families — the ones putting up with all the asinine interpretations of hastily cobbled together laws are clean as a whistle, as far as unknown positives are concerned. No wonder they’re getting cranky.
Looking for the exit
So, we’ve flattened the curve, prepped and planned the hospital response and put the economy into lockdown. Next, we need to look to an exit strategy. The political class also needs to bring the public along on this journey. Maybe a health version of Bob Hawke’s Economic Summit, done on the web, to allow for social distancing.
After some early stumbles and mixed messages by Prime Minister Scott Morrison and the Chief Medical Officer, Professor Brendan Murphy, both men seem to have gone on to do a fair job on the daily narrative.
However, the poor old punters are getting sick of being talked at by politicians who adopt different standards for themselves, or talked down to by instant experts, and the public are still going through varying stages of grief: denial, anger, bargaining, with depression to come in the next few weeks. They need help now to move on to hope and realism.
The bureaucratic bubble of the other ranks’ health boffins is a big part of the problem here.
Routinely ignored and underfunded by politicians, they’ve recently emerged from anonymity to share their time in the glare of television lights.
Their current top-down political road map seems to be at least six months’ hibernation followed by a scratch and a look around with the hope that a 100 per cent safe, effective, universally available vaccine is just around the corner. Well, unfortunately, it isn’t just around the corner. It’s not even down the road.

Jane Halton, a respected former Australian Health Department boss turned international vaccine hunter — she now chairs the Bill Gates-backed Coalition for Epidemic Preparedness Innovations — says a vaccine could be 12 to 18 months away or longer, or it may in fact never arrive. It may only last a year if it does arrive. In other words, we can’t count on it.
So, what is our plan B? You’ll be pleased to know, we officially have one, of sorts. It’s called the Australian Health Sector Emergency Response Plan for Novel Coronavirus and you can find it on the Australian Department of Health website.
From looking at the timetable in the document, we’re about to move to the targeted level of the action stage, where governments are supposed to be maintaining quality care, while communicating to “ … engage, empower and build confidence in the community”.
Hands up all of you out there who are feeling engaged and empowered at the moment.
State health departments have grudgingly started to trickle out some basic stats, but the details vary widely between the states and it’s difficult to build up a clear national picture of what capacity we have to move on to more widespread testing of priority targets, or the location and demographics of high-risk groups or industries, or whether we intend to embark on any sort of genuine random sample of tests.
We don’t know our capacity for further testing and we don’t know about the failure rate of the tests we are now doing.
Without a vaccine, testing is the only pathway to a solution that we have.

The immunity question
Former British prime minister Tony Blair last week succinctly outlined the critical decisions facing the British government, in the face of a soaring death toll. “None of the options are without problems, but it does remain crystal clear that mass testing is fundamental to exiting lockdown. Any other approach is to do this balancing act blind — a road to unacceptable loss of life or financial ruin so grave that it will crush those public services that have performed heroically in this crisis.”
In Australia, collectively we need to define our questions and quickly work towards consensus, as other countries are now doing.
The key questions are: Does exposure equal immunity? When is the end point of the illness?
How long do you shed virus particles after recovery and is this an infection risk? Is recurrence possible? How long does immunity last?
Some regions of the US and northern Italy are already looking at mass testing.
Germany is well down this path, with 100,000 tests per day. This week Germany starts new blood tests to find out who has already had the coronavirus. Tests will look for antibodies in the blood, with the aim of working out national infection rates, as recommended by the World Health Organisation on March 17.

So, what’s stopping our politicians and their boffins from starting this process here?
We reportedly have $1.5m worth of these antibody tests currently in Australia and under direction of the Therapeutic Goods Administration.
Any TGA-approved antibody tests could be trialled on the 3000-plus Australians who have tested positive for COVID-19 and who have since recovered. We already know they’ve had COVID-19 because they’ve had symptoms and tested positive to nasal swabs.
If blood tests showed they also had antibodies in their system, this may be as good as it gets for proof of immunity until, if ever, we get a vaccine.
During further random testing or mass testing, Australians could be placed into four groups.
Group 1: Antibody test positive, nasal swab negative, no symptoms. This group could include one in five Australians. Do we provide them with a COVID certificate and let them get back to work?
Group 2. Antibody test positive, nasal swab positive, with symptoms. This group has acute levels of infection and should be isolated and treated as per guidelines.
Group 3. Antibody negative, nasal swab negative, no symptoms. This group has not yet had the infection and has no immunity without vaccination. They need to maintain the current level of social distancing.
Group 4. Antibody negative, nasal swab positive, may have symptoms. At early stage of infection with no immunity. This group is at the early stage of infection and could include super spreaders. They should be isolated and treated as per current guidelines.

Doctors can fix it
At least we would know the rough ratios of these four groups within the broader population. In turn, we would hopefully be given maps and demographic profiles, so that we, the humble punters, would know the path forward for ourselves, our families and for the country, and make the best decisions.
It would be a massive effort to test the whole country and would need to be done repeatedly. Social equity and fraud risk would also need to be addressed. This would cost a lot less than the current economic measures in place and costs would gradually be “paid for” by freeing up large groups of people to work.
So which group among us does a massive effort every day to treat Australians? Your humble family doctors, folks.
We know almost 90 per cent of Australians visit their GP annually. Every day, Medicare usually funds about 423,900 GP visits. There are nearly 37,000 family doctors across Australia who specialise in diagnosis and chronic complex health conditions. They’re already triaging for the fever clinics and private pathology labs who have the required PPE.
Giving out COVID exposure certificates could become another one of your family doctor’s gatekeeper roles for commonwealth and state governments.
Family doctors already approve driver’s licences for older Australians, Centrelink certificates to access welfare, along with worker’s compensation, childcare certificates and sickness certificates, and regulate access to the NDIS.
It wouldn’t so much be a plan B, but rather 25 million individual plan Bs, directly involving you and your family doctor.
This might finally give some purpose to the national My Health Record system. The health boffins would like that. They could design the forms.
The real question is why aren’t our politicians talking to us about this now? The voters are running out of patience.
John Black pioneered election profiling in Australia in the 1970s and is a former Labor senator for Queensland. He is executive chairman of Australian Development Strategies. Dr Jeanine McMullan is a Brisbane family doctor and CEO of Health Geographics.