Coronavirus research hub: latest studies, news
As the world continues to battle the coronavirus pandemic, we bring you the latest research and studies that will help find a cure.

As the world continues to battle the coronavirus pandemic, we bring you the latest research and studies that will help find a cure. This page is edited by Tim Dodd and Jill Rowbotham and will be updated regularly as new studies are made public.
-
The price kids pay
— 29 April, 2020

Healthy levels of sleep and movement for children are being sacrificed during the COVID-19 lockdown, with rising concern about increased screen time and decreased opportunities for outdoor physical activity. Researchers from 15 countries showed that children were unable to use public parks, playgrounds, and sporting fields as frequently during isolation, because in many cases they were off limits during the period of isolation.
While the reduced activity and rise in sedentary pursuits that involved watching screens were alarming, the biggest concern was the potential for long term problems such as reduced levels of vitamin D, a deterioration in eyesight and in mental health.
Co-author Anthony Okely, from the University of Wollongong said: “Evidence shows that children are less active and more sedentary, with less consistent sleep patterns, on unstructured or non-school days (ie when they are not physically at school) than on school days.”
Read more: Promoting healthy movement behaviours among children during the COVID-19 pandemic in The Lancet: Child and Adolescent Health
-
Remdesivir drug shows promise
— April 29, 2020
Three new studies which test the experimental drug remdesivir as a treatment for COVID-19 show encouraging, but not decisive, results.
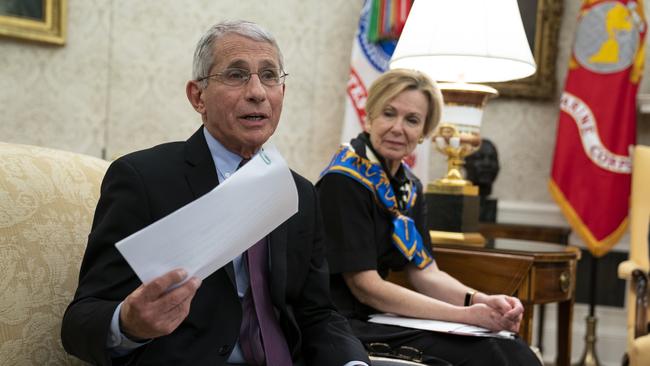
A randomized, controlled trial with 1063 patients in the US, which began on February 21, found that those who received remdesivir recovered 31 per cent faster (a median time of 11 days) compared to those who received a placebo (a median of 15 days). The comprehensive data on the study has not yet been published but Dr Anthony Fauci, head of the US National Institutes of Allergy and Infectious Disease, said at the White House: “The data shows that remdesivir has a clear-cut, significant, positive effect in diminishing the time to recovery.”
Another study of remdesivir has found that patients who were hospitalised with severe cases of COVID-19 achieved a similar level of improvement with a 5 day course of remdesivir treatment compared to those who received a 10 day course. This was announced in a media release from Gilead Sciences, the maker of the drug. The company said the data would be submitted for publication in a peer reviewed journal in coming weeks.
Finally Chinese researchers did a randomised, double-blind, controlled trial of 237 COVID-19 patients (between February 6 and March 12) which did not find a statistically significant benefit from remdesivir treatment. However it did find that patients who were treated with the drug earlier (within 10 days of showing symptoms) improved faster, but the effect was not statistically significant and the authors said it required confirmation in larger scale studies.
Read more:
Media release from the US National Institute of Allergy and Infectious Diseases, NIH Clinical Trial Shows Remdesivir Accelerates Recovery from Advanced COVID-19
Media release from Gilead Sciences, Gilead Announces Results From Phase 3 Trial of Investigational Antiviral Remdesivir in Patients With Severe COVID-19
Article in The Lancet, Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial
Very efficient transmission through air
— April 18, 2020

The Covid-19 virus “is remarkably resilient in aerosol form” and can remain infective for up to 16 hours when suspended in the air. This research found that aerosol transmission of the virus “may in fact be a more important exposure transmission pathway than previously considered”.
Studies in four US laboratories compared the aerosol transmission of COVID-19 to the 2003 SARS coronavirus and the 2012 MERS coronavirus. The short-term aerosol efficiency of COVID-19 was found to be at least equal, if not higher, than the other two viruses.
Read the research: Comparative dynamic aerosol efficiencies of three emergent coronaviruses and the unusual persistence of SARS-CoV-2 in aerosol suspensions in medRxiv.
-
Older workers risk too high
— April 16, 2020

The over-70s have been asked to self-isolate, but a breakdown in the numbers of coronavirus victims in the UK shows an alarming proportion of them are in the older worker category, the 60-69 year olds. Work by Judith R Glynn, an epidemiologist from the London School of Hygiene & Tropical Medicine questions whether the age cut off is correct, based on infection fatality rate ratios to the age structure of the population of the UK, and assuming one million infections.
It shows 70 per cent of deaths are in the over-70-years age group, but nearly two-thirds (64 per cent) of the rest occur are 60–69 years.
“This age group is not being particularly protected and includes many who are working on the frontline,” Professor Glynn argues. “Indeed, healthcare workers have even been encouraged to come out of retirement to assist.”
Those currently not working from home should be “moved to jobs with minimal personal contact, whether it is in the health service, schools, government, or the private sector”.
Read the research: Protecting workers aged 60-69 years from COVID-19 in The Lancet.
-
When the damage is done
—15 April, 2020

A substantial proportion of transmission COVID-19 probably occurs before first symptoms appeared in sufferers, concluded a new study of 94 patients at the Guangzhou Eighth People’s Hospital, that also modelled other cases. This had significant implications for controlling the highly infectious disease.
Researchers estimated 44 per cent of secondary cases were infected during the primary cases’ pre-symptomatic stage, “in settings with substantial household clustering, active case finding and quarantine outside the home”.
“Disease control measures should be adjusted to account for probable substantial pre-symptomatic transmission,” the researchers said.
Read the research: Temporal dynamics in viral shedding and transmissibility of COVID-19 in Nature Medicine.
-
The long haul
— April 14, 2020

A resurgence in COVID-19 could be possible as late as 2024, so longitudinal studies are needed to determine the extent and duration of immunity to it after the initial outbreak say scientists.
After taking into account estimates of its seasonality, immunity and cross-immunity for other viruses they project that there will be recurrent winter time outbreaks after the first wave of the pandemic has passed, so “prolonged or intermittent social distancing may be necessary into 2022”.
While expanded critical care capacity and effective treatments would “improve the success of intermittent distancing and hasten the acquisition of herd immunity”, even when the virus appears to have been eliminated, surveillance should continue.
Read the paper: Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period in Science.
–
Google ‘wash hands’ search predicts virus spread
— April 10, 2020

This study found that countries in which the term “wash hands” was searched more frequently on Google in the month from January 19 to February 18, COVID-19 spread at a lower speed in the following weeks from February 19 to March 10.
They hypothesise that the number of searches for “wash hands” not only indicates the degree of hand hygiene awareness, but might also reflect how often people wash their hands with soap, and thus inhibit the spread of COVID-19.
Read the paper: Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries in Brain, Behaviour and Immunity
–
Head lice drug shows promise
— April 3, 2020

Ivermectin, a drug commonly used to kill head lice, was found to inhibit the growth of the COVID-19 virus when tested in vitro. The authors, from Monash University’s Biomedicine Discovery Institute concluded that it “warrants further investigation for possible benefits in humans”. They stress that its use as a drug to combat COVID-19 in humans is unproven.
Ivermectin is currently used in creams and lotions for head lice and is produced in tablet form to treat roundworms.
The researchers warn that, on no account, should people self-medicate with Ivermectin because it cannot be used in humans for COVID-19 until further testing and clinical trials are complete. They also warn people not to use Ivermectin which is intended for animals.
Read the paper: The FDA-approved Drug Ivermectin inhibits the replication of SARS-CoV-2 in vitro, in Antiviral Research
–
What they knew
— April 2, 2020

Working out what the population understands about COVID-19 has been a major challenge for health and civil authorities and now an assessment of the effectiveness of rapid online surveys has revealed an interesting paradox: the public can have a good general knowledge about such a virus without understanding its implications, at least in the early stages.
In a survey of about 3000 adults in each of the UK and US conducted between February 23 and March 2, with age, sex and ethnicity calculated to reflect the distributions in each country, it was found that participants generally had “good knowledge of the main mode of disease transmission and common symptoms of COVID-19”.
However, important misconceptions included that 37.8 per cent of US participants and 29.7 per cent of UK participants thought common surgical masks “highly effective” in protecting against COVID-19. There were 25.6 per cent of US participants and 29.6 per cent of UK participants who thought it was wise to avoid eating at Chinese restaurants; and about half of US participants and 40 per cent of UK participants thought children were at an especially high risk of death when infected with the virus.
Read the paper: Use of Rapid Online Surveys to Assess People’s Perceptions During Infectious Disease Outbreaks: A Cross-sectional Survey on COVID-19 in the Journal of Medical Internet Research.
–
The enigma of kids
— April 2, 2020

Arguments about sending children back to school have made much of their lower susceptibility to COVID-19 and researchers are keen to work out why this is so.
This paper speculates that at least three elements might be having a protective effect — high concentrations of a membrane protein called ACE2; “trained” or innate immunity; and a high lymphocyte (white blood cell) count.
However it concludes that the real reasons will probably remain a mystery for the best of all possible reasons. “Fortunately … the number of infected children is too low to allow good-sized immunological studies”.
Read the paper: Will children reveal their secret? The coronavirus dilemma in the European Respiratory Journal.
–
Face masks reduce risk of infection: study
— March 29, 2020

A Chinese paper (Wiley Online Library, COVID-19: Face masks and human-to-human transmission, March 29, 2020) reports anecdotal evidence that transmission of COVID-19 is less likely if people infected with the virus wear masks. During the outbreak an infected male took public transport back to his home. On the first bus ride, lasting 2 hours and 10 mins, he did not wear a mask and five other passengers on the bus (out of 39) were infected. On the second 50 minute bus ride of his trip he did wear a mask and none of the other 14 other passengers were infected.
■ MORE: Wiley Online Library, COVID-19: Face masks and human-to-human transmission
–
Anti-malarial drug may shorten COVID-19 recovery
— March 31, 2020

A clinical trial in China has found evidence that hydroxycholoroquine (HCQ), an antimalarial drug that is a controversial treatment for COVID-19 (promoted by US President Donald Trump), could significantly shorten the recovery time for patients suffering from the virus.
The study (medRxiv, Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomised clinical trial, March 31, 2020), was carried out from February 4 to February 28 with 62 patients who were moderately — not severely — ill with COVID-19 at the Renmin Hospital of Wuhan University. The patients were randomised into a group who were treated with the drug and a control group who were not treated.
Safety of hydroxychloroquine, alone and in combination with azithromycin, in light of rapid wide-spread use for COVID-19: a multinational, network cohort and self-controlled case series study https://t.co/hlw1AbfhEN #medRxiv
— medRxiv (@medrxivpreprint) April 10, 2020
The 31 patients who were treated with HCQ (400 mg a day for five days) were observed to recovery from their high temperatures and coughs in a “significantly shortened” time compared to the 31 patients in the control group. The patients treated with the drug were also more likely to show an improvement in their pneumonia.
All four of the patients who became severely ill were in the control group which was not treated with HCQ. However two patients who were given HCQ had mild adverse reactions.
The paper follows an earlier study (Journal of ZheJiang University (Medical Sciences), A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease (COVID-19), March 6, 2020) involving 30 patients which found no effect on recovery from COVID-19 from HCQ treatment. The 30 patients, at the Shanghai Public Health Centre, were divided randomly into two groups. Each group was given the same treatments except one group received 400 mg a day of HCQ for five days. The only patient who developed severe COVID-19 was in the group which received the drug.
Chloroquine and hydroxychloroquine for the treatment of COVID-19: A living systematic review protocol https://t.co/cyxCIzJlnN #medRxiv
— medRxiv (@medrxivpreprint) April 8, 2020
Finally an article (Annals of Internal Medicine, Use of hydroxychloroquine and Chloroquine during the COVID-19 pandemic: what every clinician should know. March 31, 2020) warned that the evidence for HCQ and CQ being effective in treating COVID-19 was “limited and inconclusive”.
Because this article was published on the same day as the study (above) which found HCQ shortened the recovery time from COVID-19, the authors don’t comment on it. However they did call for more “well-performed randomised trials” test the drug.
“As of this writing, 10 such trials are under way, and information should be forthcoming within weeks,” the paper said.
–
Death rates influenced UK’s social distancing rules
— The Lancet, March 30, 2020

A paper from Imperial College London estimates that 0.66 per cent of people who are infected with COVID-19 will die, lower than has been found by some other researchers.
The new estimate comes from the team of epidemiological researchers whose work predicting high infection, hospitalisation and death rates convinced British Prime Minister Boris Johnson to make a rapid policy switch to tough social distancing rules in his country.
A new paper published in The Lancet also gives a new estimate of 1.38 per cent for the case fatality rate, that is the proportion of people who will die of those who have symptoms of COVID-19 or are otherwise confirmed to have the disease.
The two percentages are different because many people have the disease without being aware of it, and are never diagnosed.
The new paper, which is based on a wide collection of data, mainly from China, also estimates the impact of COVID-19 on different age groups.
It is hard to find the words to express my debt to the NHS for saving my life.
— Boris Johnson #StayHomeSaveLives (@BorisJohnson) April 12, 2020
The efforts of millions of people across this country to stay home are worth it. Together we will overcome this challenge, as we have overcome so many challenges in the past. #StayHomeSaveLives pic.twitter.com/HK7Ch8BMB5
The infection fatality ratio is larger for older people. For example for 20-29 year olds it is almost negligible at 0.0309 per cent. But for people 50-59 years old it is 0.595 per cent, for 60-69 year olds (1.93 per cent), for 70-79 year olds (4.28 per cent), and for those over 80 (7.8 per cent).
Case fatality ratios (the proportion of people confirmed to have the disease who die) are higher. For in and over 80s (13.4 per cent).
Estimates of the rates of hospitalisation also rose in older age groups. For people 30-39 it was 3.43 per cent, for 40-49 year olds (4.25 per cent), for 50-59 year olds (8.16 per cent), for 60-69 year olds (11.8 per cent), for 70-79 year olds (16.6 per cent) and for those over 80 (18.4 per cent)
The study concluded from its data that, based on the proportion of infected people requiring hospitalisation and the likely number of people who will be infected, that “even the most advanced healthcare systems are likely to be overwhelmed”.
■ MORE: The Lancet Infectious Diseases, Estimates of the severity of coronavirus disease 2019: a model-based analysis.
–
Mental health concerns
— The Lancet, March 31, 2020
Mental health in China significantly deteriorated during the outbreak of the COVID-19 pandemic earlier this year with levels of depression and anxiety higher than 12 months earlier.
Researchers were in the fortunate position of having down a major survey of the mental health of 101,120 people in 31 Chinese provinces in January and February 2019.

In 2020, during the pandemic, another survey was done of 8,151 people, with about 2,000 from each of four areas. One group came from of the area of the outbreak in Hubei province. There was also a high-risk area, a medium risk area and a low-risk area selected.
Overall the incidence of anxiety and depression during the pandemic was up by 15 per cent and 11 per cent (respectively) compared to a year earlier.
Not surprisingly, the impact was felt worse in areas where the pandemic was worse.
Anxiety symptoms were increased in the low-risk, the medium-risk, the high-risk and the outbreak area by 12 per cent, 8 per cent, 17 per cent and 32 per cent respectively.
Depression symptoms increased by 8 per cent, 6 per cent, 14 per cent and 24 per cent respectively in those areas.
■ More in The Lancet preprint, The impact of the coronavirus disease 2019 outbreak on Chinese residents’ mental health.
–
Don’t jump too soon
— The Lancet, March 25, 2020

One lesson from modelling data from the Wuhan lockdown may be that even a month’s delay in lifting control measures could make a worthwhile difference according to new work from the Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group published in The Lancet.
The group modelled the effect of school closures, extended workplace closures, and a reduction in mixing in the general community into the future, simulated lifting control measures by allowing a phased return to work and also examined the effects of returning to work at different stages of the outbreak (at the beginning of March or April).
“Our projections show that physical distancing measures were most effective if the staggered return to work was at the beginning of April; this reduced the median number of infections by more than 92 per cent and 24 per cent in mid-2020 and end-2020, respectively,” they concluded.

The advantage lay in “delaying and reducing the height of the peak, median epidemic size at end-2020, and affording healthcare systems more time to expand and respond”.
Limitations to the analysis included “large uncertainties around estimates of R0 (level of infectiousness) and the duration of infectiousness”.
For more: The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study; by Kiesha Prem, Yang Liu, Timothy W Russell, Adam J Kucharski, Rosalind M Eggo, Nicholas Davies, Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group, Mark Jit, Petra Klepac (The Lancet, March 25, 2020).
■ https://doi.org/10.1016/S2468-2667(20)30073-6
–
Lockdown blues
— The Lancet, March 24, 2020

Take care of the healthy too, warns research into the effects of severe confinement on the general population during the COVID-19 outbreak.
The survey of 369 adults in 64 cities in China was taken on February 20 and 21 after they had been confined for a month due to the COVID-19 outbreak.
Although there was “severe disruption” across the board, researchers found the severity of coronavirus in an individual’s home city predicted their life satisfaction, and this was “moderated by individuals’ existing chronic health issues and their hours of exercise”.
The non peer reviewed article in The Lancet by Tongji University’s Weng Fei and independent authors found 33 per cent of the participants had not left their homes during the month; 27 per cent had worked at the office; 38 per cent worked from home, and 25 per cent had stopped work due to the outbreak. “Those who stopped working reported worse health conditions… as well as distress,” the authors noted.
“We especially need to support [them]. Our results also highlight that physically active people, as indicated by more hours of exercise,might be more susceptible to wellbeing issues due to the lockdown. Policymakers who are considering introducing restrictive measures to contain COVID-19 may benefit from understanding.”
MORE AT: Health, Distress and Life Satisfaction of People in China One Month into the COVID-19 Outbreak.
–
What children can teach us
— March 13, 2020

Rectal swabs may be better than oral ones as means of judging the effectiveness of treatment for coronavirus and working out when to call a halt to quarantining. Researchers from the Guangzhou Women and Children’s Medical Centre who conducted a study on 10 children with COVID-19 between 22 January and 20 February — a time when there was very little research done on the paediatric condition — also concluded that the gastrointestinal tract may shed virus and fecal–oral transmission may be possible.
The children were identified as ‘highly suspected’ because they had had contact with someone who had the virus in the previous 14 days or were part of a family cluster.

“Compared to adult patients, the 10 paediatric patients had clinically milder symptoms and showed fewer alterations in radiological and laboratory testing parameters,” they said in the paper reported in Nature.
“For example, none showed clear clinical signs or chest X-ray findings consistent with pneumonia, a typical feature seen in the initial adult patients.”
The virus remained detectable in rectal swabs “well after nasopharyngeal swabs turned negative, suggesting that the gastrointestinal tract may shed virus and fecal-oral transmission may be possible”. But while it was possible rectal swab testing might be more useful “in judging the effectiveness of treatment and determining the timing of termination of quarantine…we do not have evidence of replication-competent virus in fecal swabs, which is required to confirm the potential for fecal–oral transmission.”
More at: Xu, Y., Li, X., Zhu, B. et al. Characteristics of paediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med (2020).
■ https://doi.org/10.1038/s41591-020-0817-4


To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout