Australia’s sleep crisis: has Flinders University cracked the code to a better night’s sleep
Medico and long-time insomniac Michael Mosley was offered a good night’s sleep as part of a groundbreaking Flinders University trial. His results have ramifications for us all.
This story was first published in February 2024. Michael Mosley passed away in June 2024 of natural causes while on a trip to Greece.
Scientist Priyanka Vandersman had always viewed her night-owl ways “as a bit of a blessing”, particularly when completing her PhD. She was working as a nurse and then staying up each night until two or three in the morning, beavering away at her studies.
The problem was, when she stopped studying and began working at a day job she simply couldn’t return to normal sleeping patterns. She had insomnia and even if she went to bed early she was still tossing and turning until 3am. She wouldn’t ever fall asleep “until my body was so overtired that it would just give up … that sense of falling asleep naturally was a struggle for me, forever”.
She was frazzled when she got up to go to work. And then she had a baby and things turned from bad to worse. She tried everything from bath salts to teas to Temazepam, but was frightened about the long-term consequences of sleeping tablets. And so when the opportunity arose to put her body on the line for science – in a groundbreaking sleep study at Flinders University Sleep Institute in Adelaide, conducted by Professor Danny Eckert and Dr Sutapa Mukherjee – she leapt at the chance. Like the 30 other chronically poor sleepers who participated, she was exhausted and had exhausted all options.
During her evaluation for the eight-week trial she was instructed to swallow a capsule that measured her core body temperature. The optimum time for deep sleep is when the body’s temperature is at its lowest. It was a measure of her circadian rhythms, her body clock. The sleep researchers discovered that her lowest temperature was around 5am or 6am.

“No wonder at 8am, when I had to take my daughter to childcare, I was very groggy,” she says. And so the sleep team worked at winding back her body clock to a more friendly hour. She met weekly with a sleep psychologist who walked her through the facts around sleep and circadian rhythms in an effort to build better sleeping habits.
Counterintuitively, she initially had her bed time restricted to just six hours in an effort to set better patterns. For a week, she was to go to bed at midnight and rise at 6am, and as soon as she woke she put on light-emitting glasses, called re-timer glasses, which mimic morning sunlight. There was no coffee after 2pm, and at night all lights were dimmed in the house an hour before sleep time, and she took melatonin.
Over the course of the eight weeks the sleep team were able to shift her minimum core body temperature, her optimum time for deep sleep, from 6am back to 2am – “which is where you want it to be because then gradual awakening would happen afterwards”. She is now getting good quality sleep most nights. It has changed her life. “My quality of life is much, much better … I wake up in the morning and I feel ready for the day,” she says. She’s more tolerant with her daughter, and her husband. She’s happier.
“I would start my day with frustration and then end my day with frustration – and that has been lifted from my life,” she says.
Good sleep is essential to our physical and mental wellbeing
Professor Danny Eckert from the Flinders University Sleep Institute steers me in the direction of a couple of human experiments to drive home his point about the importance of good sleep. In one experiment at the University of Chicago in 1999, 20-year-old college students were put in a sleep laboratory and had their sleep restricted to just four hours a night for six nights.
“At the end of the study they’d gone from being perfectly healthy to being in a pre-diabetic state,” he says. “That’s in just one week!”
In another, at the same university in 2011, young men were deprived of sleep and had their testosterone levels tracked. “In one week, it was as though they’d aged a decade,” he says of their sagging manliness.
Mukherjee, his colleague in the Flinders University Sleep Institute, cites another case to nail the issue. “We know that if we deprive rats of sleep they die after about 30 days,” she says. “They die from sepsis or infection, so we know how really important sleep is for our immune system to work.”
Deprivation of sleep is classified as torture under the Geneva Conventions, as all parents of poorly-sleeping babies can confirm. Good sleep is essential to our physical and mental wellbeing. To be deprived of it for long periods can lead to dire consequences and is a path to a premature death. That’s because sleep is when the body’s maintenance crews clock on, tending to our battered bodies, detoxifying organs, repairing damaged cells and calming restless minds. “If we were superheroes, sleep would be our superpower,” says Mukherjee.
The kryptonite, however, is modern life.
Up to 40% of Australians are not getting enough sleep
Australia is in the midst of a sleep crisis, exacerbated by our bedtime addiction to devices, which causes havoc to our circadian rhythms. Up to 40 per cent of Australians are not getting the recommended seven to nine hours of sleep a night, 15 per cent of us suffer from clinical insomnia and a further 20 per cent from debilitating, and potentially deadly, sleep apnoea – while 80 per cent of those with sleep apnoea remain undiagnosed and untreated. Yet it is an area of medical science that is poorly understood by sufferers and general practitioners. Doctors are treatingconditions such as high blood pressure, anxiety, diabetes, depression and obesity often without addressing one of the driving, underlying factors – inadequate sleep. That is something Eckert, Mukherjee and their team of sleep experts at Flinders University are hoping to change. Their clinical trial involves chronically poor sleepers who have suffered – in some cases for decades – in the grip of a maddening and constant state of exhaustion. The researchers hope their study will revolutionise the treatment of various sleep ailments.
The institute threw everything it had at solving the chronic sleep disorders of the 30 patients during the eight-week trial. A team of 60 specialist sleep doctors, psychologists, physiologists and even a specialist dentist worked on the project, to firstly diagnose and then treat the long-suffering patients. Each participant was evaluated then rigged up to state-of-the art sleep monitoring equipment in their homes, allowing the clinicians to track their progress in real time and then tailor individual treatments.
“This study was really trying to reinvent the way that we diagnose and manage sleep disorders, and do it in a revolutionary way where we try to fix them quickly,” Mukherjee says.
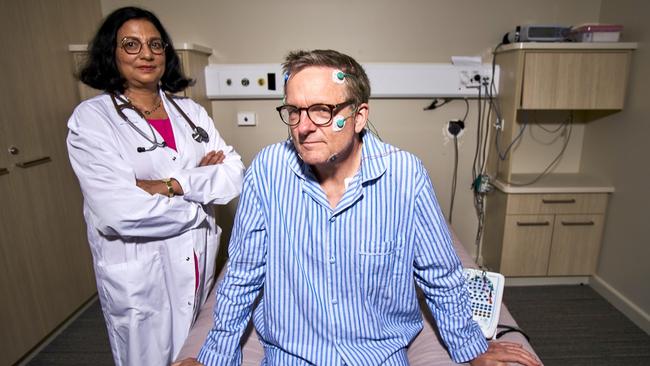
And it was all captured on film. The renowned British filmmaker, author and physician Dr Michael Mosley has made a compelling three-part documentary series about the experiment. Australia’s Sleep Revolution will be broadcast on SBS next month. Mosley, a long-time chronically poor sleeper and a participant in the trial, is a patient and the show’s narrator.


During filming, the crew flew to Canberra where they monitored various politicians, including Jacqui Lambie and Barnaby Joyce, during a gruelling two-week sitting of parliament. Their results were atrocious – long days, long nights and a lack of sleep saw Joyce’s blood pressure rise from high to dangerously high over the sitting period, placing him in the pre-diabetic range. He suffers from severe sleep apnoea. Lambie was unaware that she too had apnoea – as she said, it had been a while since she’d shared a bed with a bloke who could alert her.
“Obviously I went and saw a doctor after that and got on more pills that brought [my blood pressure] right back down,” Joyce tells me. His severe obstructive sleep apnoea causes him to stop breathing, sometimes for as long as 30 seconds, before he wakes up to draw breath. Is he going to do something about that? “No, not really, no,” says the former deputy prime minister. “Let’s cut the bullshit. I’ll just soldier on until I think I’ve had enough of this [politics], probably next term, I suppose.”
“It was an interesting exercise,” he says of the sleep study. “They tell you something you probably already know, but you hate being officially told it – which is that you’re living a very unhealthy lifestyle and if you continue on with that, it’s gonna kill you.” Days after we spoke, he fell off a pot plant in a Canberra street late at night and was filmed sprawled out on the footpath, shouting into his phone. Asked if he had anything to add about that incident, he says: “Probably not a very good idea.”

Mukherjee and Eckert say they hope to spark a national debate about sleep being one of the essential three pillars for good health, alongside diet and exercise. “I would argue that sleep is the first of those,” says Eckert. “You can’t really have the other two without good sleep.” Mukherjee says she would like to see a public awareness campaign about the importance of sleep, similar to the hugely successful “Life. Be In It” campaign which began in the mid-70s and encouraged Australians to exercise. The famous Aussie couch potato, Norm, could perhaps be rebranded as the chronic sleep apnoea sufferer, Snorm.
The treatment for Priyanka Vandersman was reasonably simple, but the correct diagnosis took years, as it did for the star of the show, Dr Michael Mosley. Having returned to England, we chat online; he’s rugged up for winter in his house on the outskirts of London. The famous documentary maker has always suffered from insomnia, but he was shocked to learn he had another debilitating and dangerous sleeping disorder, which will be revealed in the show. He is well-read and very knowledgeable, but the doctor was unable to diagnose himself.
We need 7-9 hours sleep a night
Mosley says his sleeping problems made him “grumpy and irritable and not great company when I was at home, and I felt tired a lot of the time … it’s quite lonely and boring waking up in the middle of the night and not being able to get back to sleep”. He says it probably contributed to his type-2 diabetes and with the struggles he had keeping off weight in his forties and fifties. “All these things are quite insidious, they kind of creep up on you,” he says.
What he learnt from participating in and observing the study is that while the diagnosis is quite complex, the treatments can be relatively simple. “You have to be careful about what people actually have, and generic advice is probably not going to work for an awful lot of people … we know all the simple advice of sleep hygiene, keeping your room cool and dark and quiet, but for many people it has to go deeper than that.” Mosley says he’d made programs before about sleep and therefore, “I thought I knew most stuff there was to know about sleep. I was surprised by the fact that I had a slightly faster body clock and therefore I should expose myself to bright light in the evening.” He’s been telling everyone for years that they all needed to be exposed to bright light in the morning, as was the case for Vandersman. Whereas for him, it was the opposite.
The treatments Mosley received have made an enormous difference. His wife says he’s not snoring any more and his insomnia is greatly reduced. “I still wake up sometimes at three in the morning, but I am now finding it easier to go back to sleep,” he says. “I am generally a more cheerful soul – it’s the impact on my mood which has been the main thing.”
Adelaide comedian Jon Brooks was another of the patients.
“It’s great,” he says of the change in his sleeping habits since the study. “I had a great night’s sleep last night … it’s a health problem but what I have found since the sleep study, and the treatment I was prescribed, is that my sleep does not spiral out of control.” Prior to the study, he had been a poor sleeper since “about 2010” and despite seeing many doctors his sleep apnoea was not diagnosed for years. His doctors had never taken sleep into account when diagnosing other ailments. When his son was born – the infant was “a very poor sleeper” – things started to spiral out of control. “I was getting two or three hours of solid sleep a night. It was pretty awful. I really wasn’t functioning at all.”

The first time he realised he had a major problem was when he went on tour with some other comedians and they moved their beds into the bathroom because he was snoring so loudly. They said to him, “You realise you stop breathing in the middle of the night.”
He, too, had his sleep time restricted in the study, to promote better sleep patterns and ensure that when he went to bed he was tired enough. “I wasn’t treating the bedroom where it was a haven for rest,” he says. He would often lay in bed for hours “doom scrolling” on his phone. He was also fitted with a Continuous Positive Airway Pressure (CPAP) machine to help with his sleep apnoea. It was a great success, dramatically reducing the number of times he woke through the night.
“What really surprised me about the study was that the solution to my sleep problems was staying up later until I was absolutely zonked and then getting up early … your body is something you can really tune into and you can short-circuit bad processes. You really do need to invest in sleep.” He now has good data about his sleeping habits from his CPAP machine and smart watch, something he shares with his GP. “What they are showing is I am now getting some really good sleep. I learnt from the study it only takes a small change to get big results.”
‘One step at a time’
The study was a resounding success, with more than 80 per cent of participants, long-term sufferers of insomnia or sleep apnoea or both, having had their sleep problems resolved. In a clinical sense, they no longer had insomnia or sleep apnoea. “Remember these were people with hardcore sleeping issues that had been suffering, in some cases, for decades,” Eckert says. All of the patients had a marked improvement in their sleeping habits in some way. “It is super exciting … you could actually see the difference it was making in people’s lives as the trial progressed.”
They hope the study’s success, and the documentary, will lead to more awareness about the proper treatment of sleep disorders. Eckert and Mukherjee say the growth in popularity of sleep-tracking devices such as smart watches and Oura Rings will give people a better indication of their sleeping patterns.
Mukherjee says that while these devices are “not clinical grade” they are becoming more accurate and give a good indication of how people are sleeping. “I’ve already got patients that are coming in and showing me their data,” she says. “Initially I was a little bit sceptical. But now more research is coming out, you can definitely see the strength of some of these devices.” There will come a time when this information is as valuable to doctors as blood tests and blood pressure measurements are now.
They also hope to influence the Federal Government to implement recommendations from a 2019 Parliamentary Inquiry into sleep, Bedtime Reading. Recommendations, from “prioritise sleep health as a national priority and recognise its importance to health and wellbeing alongside fitness and nutrition” to minimum standards around shift workers, were adopted by the committee. However, none have been implemented. “So there is no new money and there have been no new initiatives,” Eckert says. “The government has said it is important and we will continue to press them.”





To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout