Courage of the sister: uncovering one of medicine’s most confounding scandals
Amanda Duncan, who uncovered years of serious failings at the Launceston General Hospital, had a deeply personal reason to advocate for patients. Her sister had needed someone just like her.

Amanda Duncan felt surprisingly calm as she gathered her notes, took a deep breath, and strode into a parliamentary inquiry to drop a bombshell on a scandal-ridden Tasmanian hospital.
The young registered nurse and midwife wasn’t nervous because she was prepared. She’d spent weeks combing through coronial records, collecting allegations from fellow medical professionals, checking and cross-checking information that would shock health authorities and trouble families left questioning the death of a loved one at the state’s second-largest hospital.
Duncan was resolute as she took her seat and mindful of the impact of her revelations: “I apologise for any potential distress my statement may cause, especially to those who have lost a loved one at the Launceston General Hospital,’’ she began.
She was here, she said, to bring to light allegations of serious misconduct: the hospital’s former long-time head, Dr Peter Renshaw, had falsified death certificates. Deaths that should have been examined by the coroner had been swept under the carpet, the inquiry heard, potentially misleading families about the circumstances of a loved one’s final moments.
Duncan, the nurse-turned-amateur sleuth, had reviewed 55 publicly available coronial records of patients who had died at the LGH and collected 11 reports from doctors and nurses alleging misconduct relating to the death of a patient, including falsified medical certificates of death.
“In total there are 15 deceased patients who I am concerned may be impacted,’’ she said in her clear, firm voice.

When we speak in Hobart on a steamy February day a year on from her testimony, the Tasmanian coroner’s office is investigating the deaths of 29 patients following an independent review ordered by the state government after her evidence. Renshaw, the hospital’s former longstanding director of medical services, has denied wrongdoing.
A further 28 “inaccurately attested” death certificates have been referred to Crown Law or the Registrar of Births Deaths and Marriages.
Yet Duncan, now 30, is not satisfied. Her brave public stance cracked open pent-up suspicions and frustrations about a range of issues from families, patients and staff at the 400-bed teaching hospital. Unsure where to go with their complaints, they contact her.
The whistleblower has become patient advocate, professional confidante and government watchdog.
“I feel like I opened a Pandora’s box and I have a duty of care to see this through, for the patients, my colleagues, for the community as well,’’ she says.
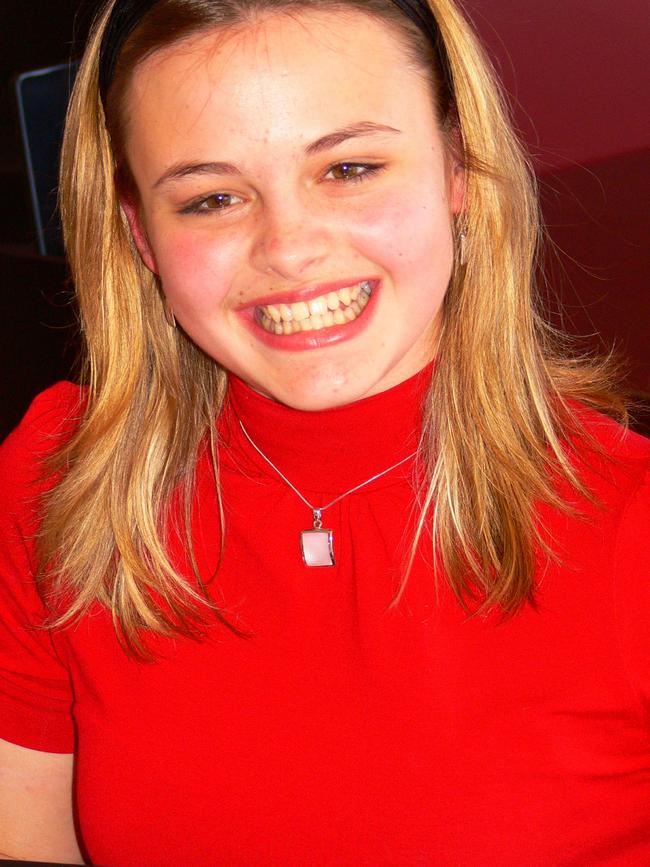
As a nurse, Duncan always felt a responsibility to advocate for patients but this struggle is deeply personal. She was just six when her sister, Zoe, then 11, revealed she was raped by a doctor when she attended the LGH with severe asthma.
Duncan watched her parents fight to be heard and for Zoe to be believed, and she saw the impact this struggle had on all of them. She understands what it is like to be brushed off, for complaints to be buried and complainants abandoned.
It motivated her to work in the health sector. “When I became a nurse, I was like, I will never be a health practitioner who will just turn my back on people who are in need in any circumstance, no matter how small,’’ she says.
When she got an inkling that death certificates were being altered and deaths hidden from the coroner, she wasn’t about to look away. She knew she had to air the allegations in a public forum to force an investigation. Last year’s parliamentary inquiry into ambulance ramping at Tasmanian hospitals came with parliamentary privilege and it was her opportunity. She didn’t miss.
“I and other health practitioners have concerns the data relating to the death and coronial investigations at the Launceston General Hospital are potentially misleading and may be skewing national data,’’ she said.
When I ask Duncan what it is like to be a whistleblower, she immediately disavows the title.
“I’m not a whistleblower,’’ she shoots back. “I’m a nurse doing her job.”
This nurse doing her job has closely watched three major probes that exposed serious failings at the hospital in recent years. She has seen the system from the inside, understands the issues uncovered in those inquiries, and has now stepped into the public sphere to fight for greater accountability and better healthcare for Tasmanians.
Duncan is speaking up because she can’t stay quiet.
“I get frustrated when our secretary of health says, ‘let’s just move forward’,” she says. I don’t believe you can move forward until you address historical and current issues, otherwise they will remain ongoing.”

Critical findings
The news was so shocking that it could scarcely be believed: a pedophile nurse had worked in the pediatric ward of LGH for 18 years, despite a litany of complaints and red flags.
A commission of inquiry into child sexual abuse found dysfunctional leadership at the hospital contributed to its failure to keep children safe from the nurse, James Griffin, 69, who killed himself in October 2019 after he was finally charged with more than a dozen offences against children as young as 11.
Griffin was not the only offender working at the hospital – the inquiry heard distressing details that a doctor had raped Zoe Duncan in 2001.
Against this troubling background, the state’s coroners had made a handful of critical findings against the hospital, highlighting serious medical failures that had contributed to poor patient outcomes and death.
Two post-surgical deaths at the hospital only made it to the coroner after complaints to the Health Complaints Commission. In one of those cases, the hospital-issued death certificate stated a 56-year-old man died of a pulmonary embolism following elective surgery. The coroner, however, found he’d died of sepsis and had not been prescribed antibiotics until shortly before his death.
“He died because of poor medical treatment,’’ coroner Simon Cooper found. “I am of the view (the patient’s) death was entirely avoidable.”
Under the Tasmanian Coroner’s Act a death must be reported after a medical procedure if it appears the death may be causally related to that procedure, and if a medical practitioner would not have reasonably expected death immediately before the procedure. Failure to comply is an offence.
Amanda Duncan was working in the operating suite and emergency department at the LGH when she began hearing doctors and nurses talking about irregularities around the reporting of deaths.
A patient’s official cause of death is not only a legal record; it also contributes to public health data on mortality rates and identifies medical errors or inadequate healthcare practices. The integrity of the healthcare system depends on transparent and accountable death reporting practices.
Aside from the corridor rumours, Duncan told the parliamentary committee she had witnessed a death in the post-anaesthetic care unit that she believed should have been investigated by the coroner.
She described how a senior anaesthetist ignored nursing requests to administer more aggressive medication to a patient who was deteriorating after a simple surgical procedure, and slapped away a nurse’s hand as she reached for the emergency alarm to call for more help.
“The in-charge nurse and I immediately escalated the situation to an emergency code blue in response to the deteriorating patient. Concurrently the patient went into cardiac arrest,” Duncan said.
After the patient’s death, Duncan said she and other nurses raised concerns, both verbally and in an incident report, that the death may have been preventable with adequate intervention. She also took it up with the anaesthetist who allegedly responded: “Peter Renshaw and I believe the patient would have died at home that day anyway. We gave the patient a kinder death’’.
Duncan said the remark had “disturbed me ever since’’.
Renshaw’s name consistently came up in her inquiries and it was a name she was familiar with after her family’s struggle to have Zoe’s sexual assault complaint thoroughly investigated.
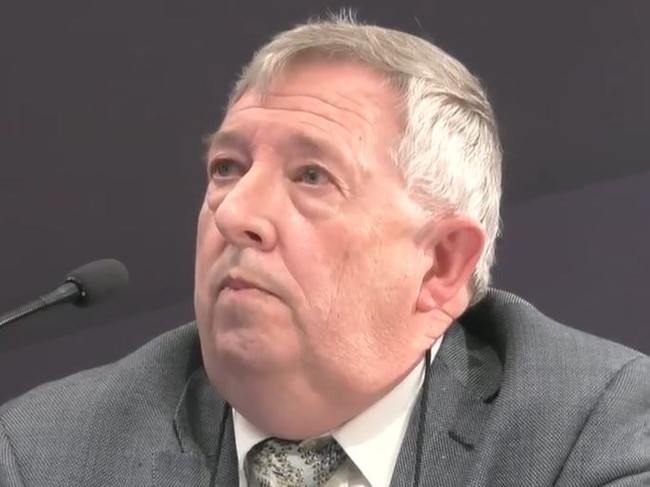
Now former junior doctors were telling her that Renshaw would attempt to coerce them into incorrectly documenting a cause of death on the medical certificate of death.
“A senior doctor reported to me the words to the effect of ‘call Dr Renshaw, he’ll fix it’, were graffitied on the laminated protocol in an acute care department,” she told the parliamentary inquiry.
Multiple nurses had told her “the only time we see Peter Renshaw on the ward was when he came to change a patient’s cause of death”.
Another nurse, Tom Millen, had come forward to the parliamentary inquiry to report that he’d been made aware of a case that should have gone to the coroner, and there had been “tea-room discussions” of more.
Months after this evidence, doctors and nurses backed it up to the ABC in Tasmania. “We were basically told, and all the junior staff knew about this, that we weren’t to contact the coroner,’’ one unnamed doctor said.
A nurse added: “We talked about Peter Renshaw’s ‘rug’, sweeping everything under the rug and how big the pile was under it”.
Renshaw’s three-decade reign at the LGH ended with his retirement in 2022, months after he gave evidence to the child sex abuse commission of inquiry which was scathing of his handling of allegations against pedophile nurse Griffin and the doctor accused of raping Zoe Duncan in 2001.
The inquiry found the response of the LGH to revelations about Griffin’s offending was passive and ineffective. Renshaw did not accept responsibility for his failures, it said. “(His) omissions and fabrications amount to misleading our commission of inquiry,’’ it added. “We do not make this finding lightly”.
It found this conduct to be unprofessional and unethical.
In relation to Zoe Duncan, it was found that he had failed to comply with the hospital’s protocol for the reporting and management of suspected child abuse.
“He did not demonstrate even a modicum of self-reflection during our hearings,’’ the inquiry found.
With her family present in the gallery, Renshaw told the inquiry that he didn’t believe Zoe’s report that she’d been raped by the doctor – only to be informed that the Child Safety Service had re-evaluated the case and found on the balance of probabilities that she had been sexually abused.
“I regret not knowing that information and I know the suggestion caused additional grief to the Duncan family, and for that I apologise,’’ he said the following day.
The inquiry noted that the doctor in Zoe’s case had been investigated for similar conduct with another patient in another jurisdiction.
Zoe Duncan did not live to hear any of this – she was reluctant to return to the LGH for treatment. She died in 2017, at the age of 28 from epilepsy complications.
Amanda still gets teary when she talks about her sister. “I remember when I rang my sister after I finished college to tell her I was going to do nursing, and she said: ‘Sissy, this is your life. Don’t do this just because of me’. And I said, ‘Don’t worry, Zoe, I’m doing this for you, but I’m doing this for others as well. This is what I want to do. It feels right’,” she says.
“Obviously I didn’t know that all this was going to happen. I thought I’d be a patient advocate by the bedside. I didn’t realise that it was going to be so public and the gravity that came out of it.’’

Scandal emerges
The Health Department had to act swiftly on Duncan’s allegations about the death certificates and an expert panel was formed to investigate.
It found significant issues in death reporting practices at the LGH, particularly concerning the actions of a former staff member, who was not named in the final report. That staff member had engaged in a “repeated pattern” of acting outside the Registration of Births, Deaths and Marriages Act and had “inaccurately” represented their standing to certify death certificates.
It recommended the former staff member be reported to the Medical Board.
“This pattern of conduct raises the issue of unsatisfactory professional conduct and whether they are a fit and proper person,’’ the panel said.
Last May, Renshaw’s registration was suspended by the Australian Health Practitioner Regulation Agency.
In January, Tasmania Police said there was insufficient evidence for any charges to be laid against Renshaw, who welcomed the move, telling local media: “I have always maintained that all death certificates issued by me or on my advice at the LGH were clinically appropriate and fully compliant with the requirements of the Coroner’s Act and the Registrar of Births, Deaths and Marriages.”
The review also identified deaths that should have been reported to the coroner, and the Coroner’s Office is investigating 29 deaths at the hospital between 2016 and 2022. The panel emphasised that referral to the coroner did not mean there was anything untoward or suspicious about the deaths, but Duncan says the ongoing uncertainty is difficult for loved ones.
“Even if the death of their loved one happened years ago, it’s like it’s happened yesterday, and it’s like they’re almost held in that state of early grief,’’ she says.
Duncan hoped the review would be the end of it but she’s pessimistic about a health system that has been plagued by a cycle of problems, reviews, and promises to fix things.
The Australian Medical Association and the Nurses and Midwives association has long flagged concerns about health staffing and retention in a state with an ageing and lower socioeconomic population base.
Duncan, who is on extended leave from her position as a nurse and midwife at the LGH, talks of the moral injury for staff working in such challenging circumstances.
“Unfortunately, we’ve lost some exceptional doctors and some exceptional nurses because they’re just sick of trying to do something and fight this system and getting nowhere,’’ she says.
Did she suffer any blowback from her revelations? “What I have done has been very welcomed by the community and the medical community for the most part,’’ she says.
She is aware that some doctors were concerned the media attention would impact the retention and recruitment of staff. “However, I don’t feel that onus is on me. I’m trying to demonstrate transparency and advocate for accountability,” she says.
The Health Department has announced a raft of reforms following the various reviews. A spokesperson said death reporting protocols were being strengthened in line with the expert panel’s recommendations. The department has also introduced new processes to deal with staff and patient complaints, which is a key priority. At the LGH, “significant changes” had been made to governance and leadership structures, including new members of the senior leadership team. “We understand that transforming organisational culture does not happen overnight and we have made significant long-term investments to improve culture across services,’’ the spokesperson said.
Duncan is sceptical that all the issues can be solved. “I don’t know that the government has the determination to review itself and its own departments in a really transparent and accountable manner,” she says.
“I get frustrated because there are all these parliamentary inquiries and independent inquiries …. and I’m like, when will our federal government step in and acknowledge this problem in Tasmania? I feel like there are so many issues, and the government is just letting it run through their hands like sand; they don’t know what to do.”
The problems don’t mean there aren’t good people in the system, or that patients don’t have good outcomes. “I hope as a nurse I have been part of those experiences,’’ she says.
“But just because some people have had great experiences, it does not detract from the negative experiences. We can’t forget about those.”





To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout