‘I was the victim of a silent heart attack’
What happened to me could happen to anyone – and they would not know about it. Silent heart attacks strike with no warning. But you can learn about prevention, and what to do next.
What happened to me was not your typical heart attack. No grasping the chest and falling down. I didn’t feel a thing.
Even more unusual was the outcome: despite permanent damage to a small section at the top of my ticker, its overall performance is still, somehow, considered normal.
Prognosis is good – as long as I keep up my fight against cholesterol, eat well, stay active and keep my blood pressure under control.
I am the victim of what is known in the medical world as a “silent” heart attack, which happens when a section of the heart muscle dies because it did not receive enough blood.
But it does so without making a fuss: no symptoms.
Silent heart attacks are surprisingly common. Harvard University’s medical school estimates they account for between 30 and 60 per cent of all heart attacks.
While the common perception of heart attacks involves sudden chest pain, silent heart attacks can take place without any pain. They can even be mistaken for heartburn.
That is why they are dangerous. One heart attack can be a warning that, if ignored, can lead to a second and potentially more serious event.
If that first heart attack is “silent”, like mine, you might never know it happened and that means you might never get a chance to take the remedial action that could prevent a second and potentially deadly episode.
While I suffered no symptoms, a battery of tests and one truly stomach-churning procedure has left no doubt that part of my heart is now a passenger.
It just sits there showing up as a dark shadow on ultrasound scans.
The first time this happened, it triggered an ominous silence from the previously chatty nurse who scurried away to report what she had found.
She returned with a warning to avoid exertion until I saw the cardiologist down the hall two days later.
That should have put me on notice that something was awry. But it didn’t. I had been haunting the local gym, was delighted with the results and considered myself to be the picture of health.
I felt better than I had in years.
It therefore came as quite a shock when my cardiologist explained that part of my heart had given up the ghost. The next step would require a surgical procedure that sounded ghastly.
Some sort of tubular probe was to be inserted into a vein in my arm, then manipulated into my heart’s blood vessels to assess the extent of the blockages that had caused the damage.
If the blockages turned out to be too extensive to be treated with drugs, the probe would insert tiny “stents” inside the blocked blood vessels and these would then be expanded to ease the constriction.
He even had a sample to show me. It looked a bit like a small mesh tube made out of something that bore a worrying resemblance to tiny, high-tech chicken wire.
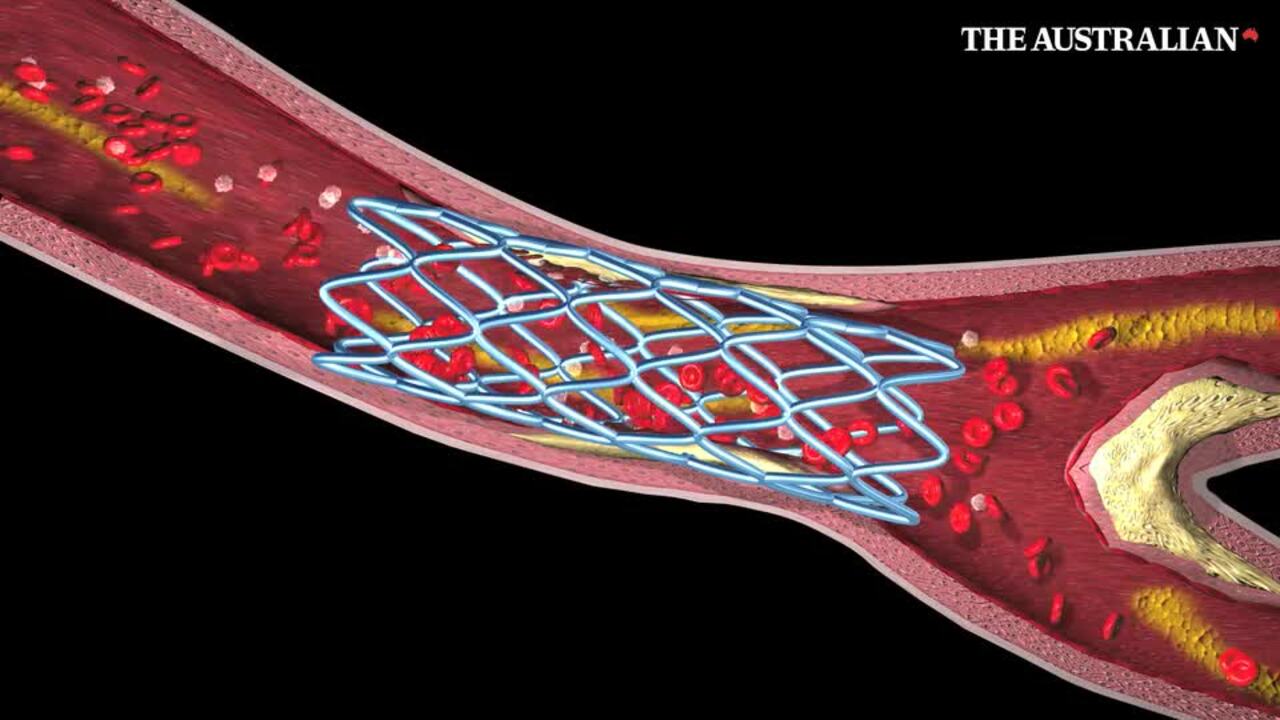
For quite a while, my response was stunned silence. I’m still not sure what was worse. Was it the prospect that chicken wire was about to be inserted into my heart? Or was it the realisation that I was not, in fact, immortal?
The only positive note, if you can call it that, was that this would all be done under anaesthetic and the tube would be inserted through one small incision near my wrist.
How could this be? My health regimen, which seemed to be working, had been aimed at avoiding exactly the sort of diagnosis that was now staring me in the face.
I had signed up with a personal trainer, had radically changed my diet, was averaging 10,000 steps a day, had shed 10kg in 10 months and had even managed to bring my blood pressure back to reasonable levels.
I took blood pressure readings every day or so, had invested in a high-tech bathroom scale and was now adept at running not just the Apple health app, but the slightly more elaborate Withings health app.
Under the watchful eye of my personal trainer, health and fitness had taken on renewed importance. And this was my reward? It seemed so unfair.

After the initial shock, I slowly began to put things into perspective. Yes I’ve had a heart attack. That can’t be changed. I’m still here. I’m not incapacitated and I’ve had the good fortune to be made aware of a serious problem that would otherwise have gone undetected.
I have also come to terms with the fact that there is a price to be paid for a lifetime of high-pressure, sedentary work accompanied by long hours, little exercise, poor diet and too much coffee.
My fitness level is fine now, but that was not the case in the past. And it’s in the past that the damage was done.
I had that surgical procedure a little over three weeks later and it went much better than expected.
The last thing I remember before the drugs kicked in was having my right arm strapped securely in place for the probe.
Above me and to the left was what appeared to be a large television screen that looked set to monitor the probe’s location as it moved up my arm and into my heart.
When I awoke in recovery it was to learn that the blockages in the blood vessels were so mild they did not need stents. So no chicken wire. Just a sore arm that was back to normal in a few days.
I was back home the same day and the only reminder of the procedure is a tiny scar on my wrist.
Instead of permanent inserts in my heart I’m now on very high doses of anti-cholesterol medication and a diet that is not too different to the regime that had been put in place a year ago by my personal trainer.
Cholesterol-clogged arteries, high blood pressure and obesity are three of the biggest risk factors for heart disease. But they can be treated with diet, exercise and drugs.
My diet now is close to what is generally known as the Mediterranean diet: lots of salmon, plenty of greens, a little lean red meat, minimal carbohydrates, no butter, low-fat dairy, plenty of fruit, almonds and flax seeds in smoothies and no more than two coffees per day.
All that is in line with the hundreds of articles and videos to be found online. But for real expertise it is worth paying for the special reports on cholesterol and blood pressure published by the Harvard Medical School.
Harvard’s cholesterol report in particular has an extensive list of foods to eat and those to avoid. Those to avoid include processed meat, highly refined and processed grains and sugars and sugary drinks.
All my work at the gym has not been wasted. My blood pressure medication has been halved and I’m back pounding the footpaths.
I’m not quite back to 10,000 steps a day but I’m getting there.
But for a series of very lucky breaks this could have been a great deal worse.
The first piece of luck was discovering the damage to my heart in the first place.
This was entirely due to the fact that I suffered two episodes of dizziness at the gym just a few days apart. I had been inclined to put it down to over-exertion but my personal trainer insisted I get to the doctor.
Lesson one: if you are serious about getting fit, invest in a personal trainer who knows what he or she is doing. It might save your life.
While my cardiologist was unable to pinpoint exactly when my heart attack happened, he was able to determine that it did not coincide with those two episodes of dizziness at the gym. The damage could have been with me for years.
The next piece of luck was that I had a regular check-up scheduled with my cardiologist just a few days after my initial visit to the GP.
My GP wanted his opinion on whether it was time to cut back on my blood pressure medication because of my weight loss and exercise regimen.
Lesson two: If you own a good car you would not think twice about spending some time to find the best service centre. Adopt the same approach with your body.
Don’t wait until something goes wrong. Adopt the precautionary principle and assemble a good health team to cover all the bits and pieces that need regular attention – just as you would with a decent motor vehicle.
And if you can afford it, don’t dump your health insurance.
In my case the greatest piece of luck was when my wife signed me up with that personal trainer. But for that, the damage to my heart might never have been identified.
The only real tragedy in this whole business is that a bottle of very expensive whiskey that I was slowly working through was destined for the Christmas cake.
Never rely on Dr Google for heart health
It’s all too common for people to joke about how they managed to diagnose their own health issues with online assistance from “Dr Google”.
That needs to be recognised for what it is: a joke.
When the chips are down, my experience proves we have a public health system in this country that is fast and efficient.
And the frontline of that system is usually your local GP.
Online gurus might know all sorts of interesting facts about cardiac infarction – which is the technical term for a localised area of dead heart tissue that results from disruption of the blood supply.
But your local GP knows something far more important: you.
My GP, Eric Barlow, tracked my adventures with cardiac health ever since I turned up in his office still thinking I was fit as a flea.
“It’s estimated as many as 30 per cent of all infarcts are silent,” he said.
“This is concerning for two reasons. One is that these silent infarcts are not being treated in the acute phase so they are at higher risk of causing complications such as abnormal heart rhythms or heart failure.

“The other concern relates to the fact that silent heart attacks are still caused by diseased coronary arteries like symptomatic heart attacks.
“It doesn’t matter if that infarct was silent. What you need to do now is secondary prevention. You can’t change the past but as studies consistently and repeatedly have shown you can dramatically lower your future risk by paying attention to all the modifiable risk factors – blood pressure, cholesterol, heart rate, blood sugar and very importantly lifestyle factors – stop smoking, eat well, get to a healthy weight, and exercise.
“People who have been diagnosed as having had a previous silent heart attack are often fearful of exercising as they worry they might trigger further damage, and be unaware of it like before.
“Perfectly understandable and a good reason to check out heart function before enrolling in an intensive training program.
“But remember – there’s no way of knowing when that silent heart attack happened, and the benefits of exercise post-infarct are without question.
“So once given the all clear, patients will be directed to improve their level of fitness including aerobic exercise, strength training and flexibility. The sooner the better,” said Dr Barlow.
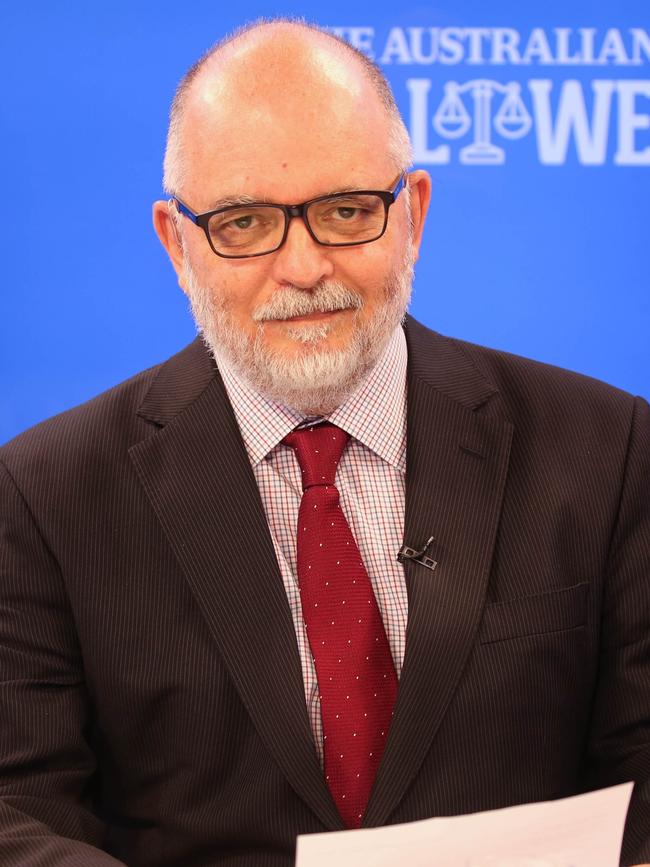
Chris Merritt is vice-president of the Rule of Law Institute of Australia.





To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout