This was, in many respects, a crisis waiting to happen. Thanks to rising life expectancy, the population requiring some form of aged care has increased relentlessly.
However, successive governments, mindful of the fact that more than 70 per cent of the costs of residential aged care are borne by taxpayers, have been reluctant to expand the number of places, and hence aged care’s overall funding, in line with the underlying growth in demand.
The result is that aged-care funding per potential user has almost halved in real terms over 25 years.
No doubt, the impacts of that reduction have been cushioned by the much greater ability of older Australians to access care in their home, with a rising share of the elderly deferring or avoiding entry into residential facilities.
However, the corollary of that trend is that those actually entering residential care are far older and in far poorer health than ever before.
Traditionally, aged-care homes catered primarily for elderly widows suffering from frailty and loss of mobility, and whose main requirement was for low-level assistance with the activities of daily living. Now, however, more than half their population is composed of residents with dementia, who have very substantial needs in terms of personal care and supervision, with a large share of the remainder being made up of residents who are at the end of life, and who require myriad forms of palliative care.
The unsurprising result of the sweeping change in their population is that the proportion of residents assessed as needing complex care has risen from 13 per cent in 2009 to 52 per cent last year, while those requiring care at its highest level has soared from just 4 per cent to more than a third.
Compared with the homes’ previous population, serving those groups is inherently costlier and more labour-intensive. But with its finances under extreme pressure, the sector has struggled to secure the workforce it requires.

The enormous expansion in the NDIS has compounded the difficulties: in simple terms, workers with similar qualifications earn at least 25 per cent more in jobs funded by the NDIS than they do in aged care. As that competition has played itself out, aged-care homes have had to rely on a workforce which is less well trained, experienced and stable than it used to be.
The sector’s structure makes the problems that creates more acute. In 2004, the Hogan report found that many aged-care homes were too small to achieve economies of scale and could not justify relying on full-time staff for activities such as nursing, cleaning and personal care.
Despite considerable consolidation, small or mid-sized homes still have a significant presence, thanks partly to regulatory arrangements which impede structural change. The result is that many of the sector’s workers split their time between several homes, making those homes especially vulnerable to community transmission of infectious diseases.
In theory, quality regulation should mitigate the risks all those issues pose to the standard of care. However, today’s funding levels provide for barely 30 minutes of nursing care, and 2.5 hours of personal care, per resident each working day, and for much less than that during the weekend, preventing homes from meeting their clients’ increasingly complex needs.
At the same time, the heavy-handed regulation to which the sector is subject is seriously flawed, offering no rewards for good performance while threatening penalties for poor performance — notably, forced closures — that are so draconian, and so costly to implement, as to be of little relevance.

To make matters worse, much of the regulation is administrative, involving a great deal of reporting and little actual surveillance. Since residents themselves are often unable to monitor the quality of care, and their families may hesitate to complain for fear of being viewed as troublemakers, appalling lapses can go undetected.
Given those weaknesses, it is a testimonial to the sector’s overall professionalism that the pandemic has been better contained than in Europe and North America, where many aged-care homes have lost a third of their residents. There are nonetheless serious concerns which must be addressed.
The most urgent task is to reduce the likelihood of infection and to respond more promptly to outbreaks when they occur. Those risks are largely being managed through lockdowns; however, the European experience shows that unless any infected residents are rapidly transferred to hospitals, the lockdowns — which are deeply traumatic for residents and their families — can become death traps. The reluctance of state governments to accept and facilitate those transfers is inexcusable.
The longer-term issues are no less daunting. It is an illusion to believe we can do without residential care. On average, providing around-the-clock assistance in the home for a person with middling to high care requirements costs $400,000 a year — and more than that for those with the severest forms of dementia. An institutional setting is therefore the only realistic option for the growing numbers who suffer from conditions such as Alzheimer’s disease.

There is also a spiralling need for end-of-life care, not merely because of population ageing but also because of the phenomenon demographers refer to as the “compression of mortality” — the tendency, as life expectancy rises, for the members of each cohort to live until about the same age and then die pretty much at once.
As a consequence of that trend, rather than experiencing deaths that are relatively spread out over their final decades, the baby boom cohorts, which are very large in absolute terms, will enter the end-of-life phase as a succession of massive, tightly bunched, waves, imposing enormous stress on the aged-care system.
If the system is to cope, almost every aspect of its structure needs to change; additionally, the sector’s overall funding must rise, potentially by as much as 0.5 to 1 per cent of GDP.
However, it is in the nature of aged care that any change must be phased in carefully, avoiding unnecessary disruption to a population that has to remain largely in place. And underlining the importance of caution, the errors made in the deployment of the NDIS and of the increased spending on mental health are stark reminders of the risks involved in overly ambitious attempts at wholesale transformation.
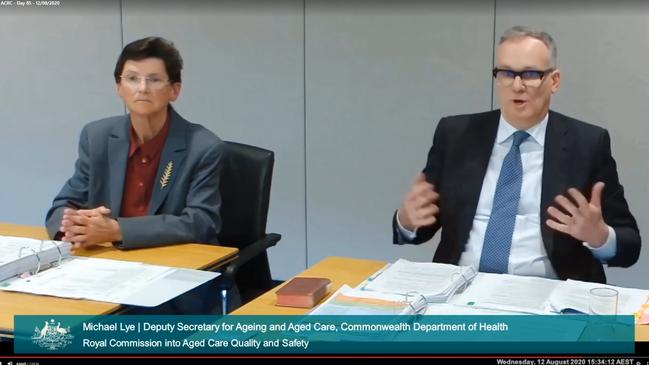
That is the conundrum facing the Royal Commission into Aged Care Quality and Safety, which is due to report in February — how to combine far-reaching reform with gradualism, predictability and affordability. If it can square that circle, it will have been well worth the wait.







As our aged-care homes battle COVID-19, the sector’s longstanding problems have come dramatically to the fore.