
You might have heard of the coronavirus’s distinctive spike protein. This is the part of the virus that attaches to a receptor on the outside of the body’s cells, allowing the virus to enter the cell and cause infection. Covid-19 vaccines work by giving instructions to our body’s cells to manufacture the virus spike protein, triggering an immune response very similar to the one that would happen after natural infection.
Depending on whether you are getting Pfizer or AstraZeneca, it will either be mRNA encased in lipid nanoparticles, or DNA in an adenovirus vector, that will deliver the genetic instructions or material that triggers production of the spike protein. Once the vaccine enters our muscle cells, they begin to produce the spike protein, and some of the protruding spikes become expressed on the surface of the cell.
“When you have the spike protein expressed on the surface of the cells, it basically sets off an alarm in the body,” says Stuart Tangye, a professor in immunology at the Garvan Institute. “It starts ringing a bell and you start having different types of immune cells travel to that site of vaccine injection … they capture the spike protein and then transport it to your lymph nodes … where all the immune action happens.”
Inside the lymph nodes, the first immune cells that get to work on the spike protein and protein fragments are antigen-presenting cells. One of these is called a macrophage. “The macrophages are big eating cells. They spot the rubbish and engulf it and, a bit like a garbage truck, break it down into small bits and pieces. Then the macrophages and other antigen-presenting cells use those bits and pieces to present parts of the spike protein to T cells and B cells, alerting them as to exactly what the invading protein or microbe is.”
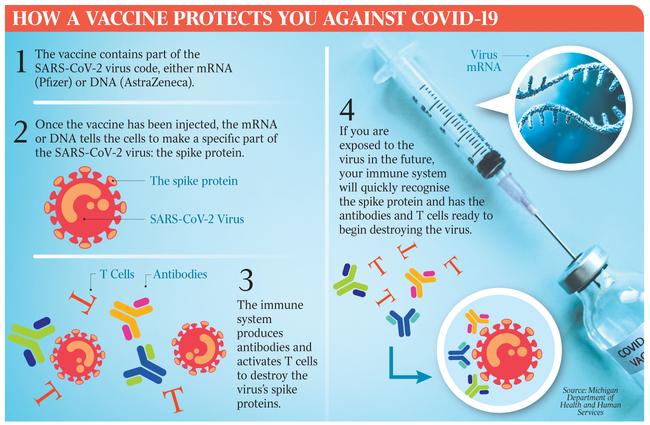
The role of B cells in the immune response is to manufacture antibodies, crucial proteins that can block the virus from invading the body’s cells. In SARS-CoV-2, when a person is infected, antibodies produced following vaccination bind to the spike protein and prevent it from being able to bind to the receptor that allows the virus to enter our cells.
Immune cells called helper T cells help activate the B cells, triggering them to produce large amounts of antibodies that target the spike protein. At the same time, antigen-presenting cells activate another type of immune cells, killer T cells, which seek out and destroy coronavirus-infected cells that display the spike protein fragments on their surfaces.
As well as flooding the body with antibodies to SARS-CoV-2 and activating helper and killer T cells, a process of immune memory is also triggered, in which memory B cells and memory T cells are formed, which retain information about SARS-CoV-2 that may trigger an immune response long after antibodies in the blood have diminished.
The level of antibodies diminishes over time, meaning booster shots will be necessary.
The immune process begins to ramp up over a few weeks after the first shot, but it’s not until the second shot that the antibody production really kicks into gear.
About two weeks after your second shot, full immunity will have been realised.




You may have had your Covid-19 vaccine, or are soon to get it. You probably had a bit of a sore arm, perhaps with noticeable swelling at the injection site. But what goes on inside the body after a vaccine is injected into the muscle? How exactly does a vaccine give us immunity to coronavirus?