Key to treating Covid-19 will be found in our DNA
Understanding why we have such varied immune responses is the most powerful tool for developing effective treatments.
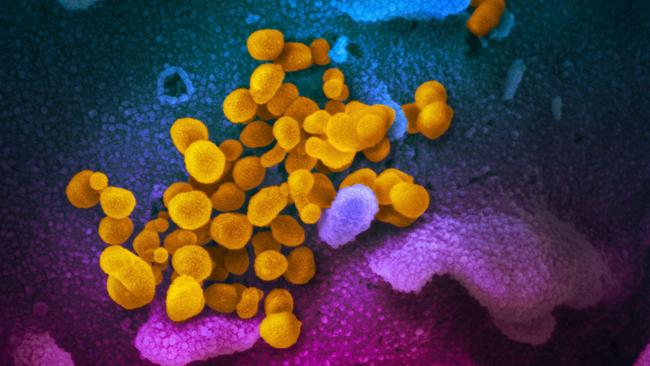
Many of history’s great plagues stem from microbes that leapt from animals into humans. But their severity is based on our individual immune reaction.
Each of us has six billion letters in our genome and, between any two individuals, there are three million letter differences. These variants are what make us unique and can also significantly change how we respond to pathogens such as viruses.
Take the Epstein-Barr virus, which causes glandular fever and is estimated to affect 90 per cent of the world’s population. In most people, the virus replicates at low levels and persists asymptomatically for much of their lives – the immune system strikes the right balance between responding to and tolerating the virus.
But in people who inherit a harmful variant in the SH2D1A gene, the same virus triggers a lethal immune response. Professor Stuart Tangye and colleagues revealed that individuals with these gene variants develop a vicious cycle of uncontrolled viral replication and ineffective, pathological immune responses and, some, a “cytokine storm”– a life-threatening immune reaction that has also been observed in patients during this pandemic.
We have hundreds of genes essential for our immune system to mount an effective response to pathogens – and a single letter out of six billion can completely throw it off balance. Our challenge is to find the variants that predispose individuals to severe COVID-19.
The human immune system may have encountered the new coronavirus only eight months ago but it has been finetuning for hundreds of thousands of years. We’re beginning to understand how.
For example, last year researchers at the Garvan Institute discovered a variant of the gene TNFAIP3, which is common in Indigenous Australians and people throughout Oceania, heightens immune responses. This TNFAIP3 gene variant traces back to an extinct human species, the Denisovans, and was likely beneficial to survival after modern humans migrated across the Wallace line in Southeast Asia to live among Australian fauna and flora 60,000 years ago. It is likely that people encountered new viruses from the Australian fauna, and surviving these may have called for less tolerance and heightened immune responses.
Bats, often the origin of virus epidemics, seem to have taken the opposite path: their immune response genes are radically altered in favour of tolerating virus infections. Bats appear to carry and shed the precursors of the coronaviruses that cause SARS, COVID-19 and MERS without it making them sick. This is an experiment of nature that points to how we might prevent severe COVID-19 disease in people. We need to use genomics to understand how what is good for a bat may be good for us too.
The crucial difference between now and even SARS 17 years ago is the extraordinary progress in DNA-based technologies, allowing us to uncover the mechanisms governing immune responses and disease. Today’s crisis shines a beacon on the urgent need to understand and leverage the “known unknowns” of immune response variability, because it has the potential to be our most powerful guide for targeted therapy – treatments that target immune molecules at the cause of excessive immune responses.
We need to know which immune response molecules are critical for controlling virus replication. We need rigorous cause-and-effect evidence: we can’t afford the time and cost of trial-and-error best guesses.
We urgently need the complete list of DNA differences for many thousands of people who have tested positive for COVID-19, from genetically diverse populations, so experimental studies can focus on differences that appear causal for extreme disease or for asymptomatic “elite resistors”. This is under way. This is an approach we know works.
In individuals suffering from atherosclerosis, an inflammatory disease of heart blood vessels, gene sequencing of people with lower cholesterol revealed some carried a DNA variant that inactivated the PCSK9 gene. This led to human monoclonal antibodies that lower blood cholesterol as effectively, and more specifically, than the widely used statin drugs.
Equally, rock-solid genetic information will lead to drugs to stop people from developing the severe immune reaction to COVID-19.
Even if a vaccine proves elusive, targeted treatment harnessing antibody genes and other immune genes will keep people out of hospital and ICU, and help tame this global crisis.
In the meantime, we at Garvan are working to bypass the complexities and variability in our body’s immune system by focusing on developing reproducible, targeted drugs against the new coronavirus.
The antibodies made by people with COVID-19 or by vaccination may be too weak and too cross-reactive, but antibody gene engineering bypasses these problems.
Monoclonal antibodies, produced in the lab, could circumvent the genetic variability of people’s own immune responses and be given to provide immediate immunity, both for the treatment of COVID-19 and for prevention, to at-risk individuals, including the elderly, chronically ill and health workers on the frontline.
Australia has a depth of expertise to mobilise therapeutic monoclonal antibodies against COVID-19 that’s second to none, thanks to the generations of world-leading Australian scientists who have built upon the pioneering antibody and tolerance research of Nobel laureate Macfarlane Burnet, Frank Fenner and Gus Nossal, the pre-eminence of CSL as a global antibody business, and decades of government and commercial investment in immunology research and national facilities. This should be a public priority.
Christopher Goodnow is executive director, Garvan Institute of Medical Research; director, Cellular Genomics Futures Institute UNSW Sydney; and a member of the US National Academy of Science.



Science is coming to grips with the key question in the COVID-19 crisis: why do some of us develop severe disease requiring intensive care while others have mild or asymptomatic infections? The solution to that question is not in the virus itself, it’s in the way our immune system reacts to the virus.