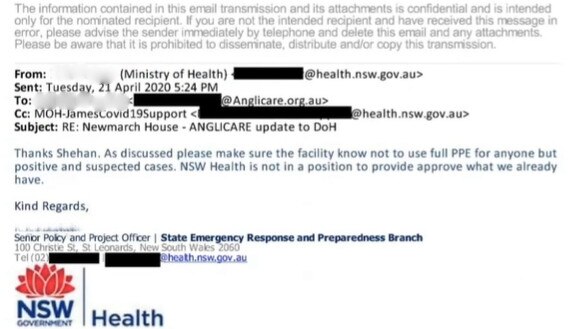
‘Deeply distressing’: NSW Health email told Newmarch House not to use PPE around all residents
A bombshell email shows coronavirus-stricken Newmarch House was given a shocking piece of advice at the peak of the pandemic.

NSW Health told staff at coronavirus-stricken Newmarch House not to use PPE unless they were around aged care residents who had tested positive or were showing symptoms, the aged care commission has heard.
The stunning revelation came in an email tendered to the Royal Commission into Aged Care on Tuesday, which was sent from the NSW State Emergency Response and Preparedness Branch to Anglicare, which runs Newmarch House.
The email said: “As discussed please make sure the facility know not to use full PPE for anyone but positive and suspected cases. NSW Health is not in a position to provide approve (sic) what we already have.”
Anglicare chief executive officer Grant Millard said the policy was “deeply distressing” because it contradicted expert advice they were receiving from head of infectious diseases at Nepean Hospital James Branley, who was working closely with Newmarch House.
The advice was for all care workers to wear PPE around all residents.
Mr Millard said the lack of PPE likely contributed to their workforce issues, which resulted in them standing down 87 per cent of their regular staff and many members of their surge staff “very early on” because they were close contacts of COVID-positive people.

“The advice of the expert we had (was) that you really need to treat all of your residents as COVID-positive until it’s proven otherwise through multiple rounds of testing over a designated period,” he said.
“That made sense, and I think that was our experience – that many of the residents were still incubating.
“An inadequate supply of PPE upfront meant that many of our staff were either infected or listed as close contacts.”
Mr Millard said Anglicare had found sourcing PPE to be “incredibly challenging,” including when trying to source it from the federal government.
“There was a lack of clarity about PPE access pathways at both state and federal level, no co-ordinated or centralised contact point and challenges in continuity of access and timely delivery,” he said.
“Our staff were being instructed by Dr Branley to utilise full PPE for all Newmarch House residents.
“But we encountered contrary views when we sought access to the national PPE stockpile.”
‘NOT UP TO THE TASK’
After Newmarch House lost the majority of their staff to isolation, the federal government provided them with an online platform to use that could supply replacement staff, called Mable.
But Mr Millard said Mable provided “very few people who had any residential aged care experience,” adding that “early on, they just weren’t up to the task.”
He said this improved over a period of weeks – but at the critical early juncture, the replacement staff were working with little skills or training in aged care during an outbreak.
“It was dangerous to them,” he said.
A Mable spokesperson said in response, “On receiving this feedback and observing the challenges that were being faced, Mable responded by tailoring its platform and processes to the needs of Anglicare, including by developing new search and screening criteria to help Anglicare identify suitable workers that met their requirements.
“This was fully operational within just a few days of receipt of the feedback provided by Anglicare to Mable. This explains Mr Millard’s comments today that ‘we were supplied by some very capable people’ once ‘the requirements and specifications for the particularly challenging environment were better understood.’
“Workers were subsequently engaged by Anglicare via the Mable platform until the end of June 2020.”
HOSPITAL TRANSFER KEY ISSUE
One of the core subjects of Mr Rozen’s questioning of the Anglicare leadership was the decision for the majority of Newmarch House’s COVID-positive patients to be treated in a ‘Hospital in the Home’ approach within the facility, rather than be transferred to actual hospitals.
The commission heard on Monday that NSW Health had a “preference” for Newmarch House residents not to be transferred to hospitals because it didn’t want to “set a precedent.”
The question of hospital transfer was one of the causes of “robust” discussions with “a frustrating level of dysfunction” and “conflicting advice” between Anglicare and the state and federal governments, Mr Millard said, which were “particularly intense in the first two weeks of the outbreak.”
Mr Millard said in hindsight, he should have stood up to the government and pushed for COVID-positive residents to be transferred to hospital.
“In the event of infection at another home, Anglicare would be far more assertive regarding the most appropriate management of COVID-19 positive residents and would strongly push for these residents to be immediately transferred to hospital,” he said.
“The understanding was” that it would be possible for COVID-positive residents to be transferred to hospital “if it was clinically indicated that they would benefit from being transferred to hospital,” he said, but this is not what eventuated in practice.
He said residents remaining in the facility presented a “monumental challenge” in containing the infection and keeping other residents and staff safe.
“(Not transferring COVID-positive residents to hospital) really had an impact on all the residents, who were still confined to their rooms,” he said.
“I believe that if we would have been able to transfer COVID-positive patients earlier, we would have had an earlier liberalisation of what was really difficult for our residents to go through: being isolated in their rooms with their doors closed.“
Mr Millard said residential aged care facilities were not as equipped to deal with acutely unwell patients, or an outbreak of an infectious disease, as hospitals.
“It’s just not the way an aged care home operates,” he said.
“My understanding is that on average, the funding for an aged care resident per day is something in the order of $250 to $300 … versus someone in a hospital, certainly in acute, would be in the order of at least $1200, $1300 a day. Those numbers are approximate.
“It’s not reasonable to anticipate any of that level of equipment and resourcing will be available in a residential aged care home, as it would be in a hospital.”
Of the 97 residents at Newmarch House, 17 died of the coronavirus.
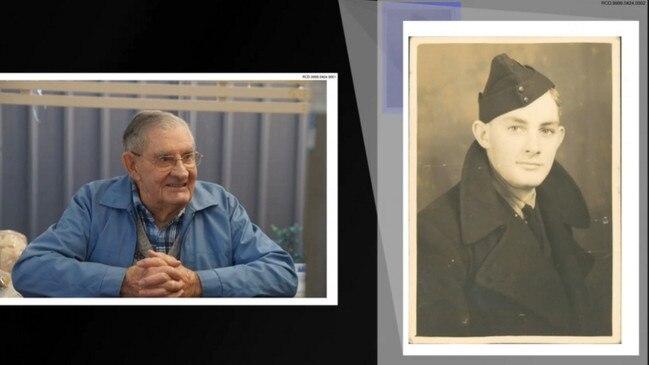
EARLIER: ‘I RANG EVERY DAY’ AS DAD WAS DYING
A woman has shared heartbreaking testimony of her father dying in Newmarch House, the site of a tragic coronavirus outbreak in Sydney this year.
Virginia Clarke spoke to the Royal Commission into Aged Care on Tuesday about her experience with Newmarch House, under questioning from counsel assisting Paul Bolster.
She said was left in the dark as her father tested positive and then died of COVID-19 in April this year.
She found out he had tested positive to the coronavirus in a confronting phone call from a woman who thought she would have already been informed.
“You don’t know?” the woman said to Ms Clarke.
“I’m really sorry to have to tell you, but he’s tested positive for COVID-19.”
“I was in shock – I didn’t know what to say,” she said.
“I asked her some questions – she was in a bit of a shock as well, because she thought I already would have known. And that was it. We didn’t get anymore information from her, or from anyone else.”
Mrs Clarke said staff would not tell her if her father himself had been informed he had tested positive to the coronavirus.
“I don’t know that he knew that he had tested positive to COVID-19,” she said.
“I don’t know if he knew he had COVID-19 or not.
“I didn’t want to upset him by telling him that he had tested positive if he didn’t already know.
“I thought that somebody should have told him, or if they wanted me to tell him I would have wanted somebody with him. Because he would have asked me what was going to happen. Well, I don’t know dad.”
Ms Clarke’s father had been happy in Newmarch House up until March, when everything changed.
The centre went into lockdown around March 23, and she was not able see her father after that.

Ms Clarke said at the start of the outbreak she “rang every day to find out what was happening.”
“Sometimes I would get a phonecall back, sometimes I didn’t,” she said.
She said “there was no discussion” about him being transferred to hospital.
Mrs Clarke voice cracked as she told the commission how she was asked to fill out an end-of-life form by the centre without being able to speak to her father first.
Newmarch House staff eventually allowed her to speak to her father on the phone while she filled out the form with him.
There was “nothing whatsoever” from staff to indicate to her that her father was likely to die – until he passed away on April 19.
There was one further heartbreak for Mrs Clarke – she was delayed from saying goodbye in a funeral because there was no time of death provided with his body from Newmarch House.
“I tried to contact Newmarch House and could not get an answer to a phonecall, so I had to estimate his time of death so that the crematorium would accept his body,” she said.
Ms Clarke said she was calling for better training, better access to doctors and nurses for aged care residents, and better communication, among the lessons to be learned from her experience in Newmarch House.
“Our elderly need to be protected,” she said.
“It’s not fair what happened to my dad at Newmarch House.”
Newmarch House was the site of an outbreak with 17 deaths from COVID-19 in the first wave of the virus.
MINISTER DEFENDS ACTIONS
Federal Aged Care Minister Richard Colbeck has defended the government’s handling of coronavirus in residential aged care facilities saying it provided a “very comprehensive document” with a range of measures for managing outbreaks in March.
He said the advice was updated in April, and again on July 14.
“I just want to put on the record, we have worked extremely closely with the sector,” Mr Colbeck said.
“We have been meeting on a very regular basis, weekly, sometimes twice-weekly, to ensure they were informed of what we were doing.
“We were learning from their experience, and interacting with them on a regular basis to understand the concerns that they might have, and how we might act on those concerns, and how we might continue to build the plan that we have for COVID-19 in residential aged care.”


