THE Territory has the nation’s highest rate of STIs. We’re more likely to get gonorrhoea, syphilis and chlamydia than people living anywhere else in Australia.
That in itself isn’t new news.
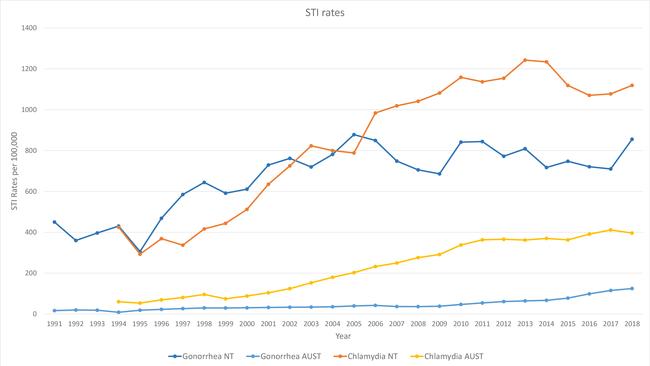
The Australian Government’s national notifiable diseases surveillance system tracks back to 1991, and early figures show STIs have always plagued Territorians at a rate disproportionately higher than the rest of Australia.
Then, there were 450.2 notifications of gonorrhoea for every 100,000 Territorians — more than 26 times the national average.
In 2018, more people tested positive to gonorrhoea in the NT than any year on record — and per capita, Territorians were 6.8 times more likely to get the infection than people living anywhere else in Australia.
When the Commonwealth started recording chlamydia notifications in 1994, Territorians were seven times more likely to have the disease than other Australians.
Now we’re only twice as likely to get it compared to other Aussies but that’s not because our rates have gone done. Instead the disease has become more prevelant across the entire country.
And as health experts scramble to control the epidemic, Australian politicians are simply pointing their fingers at each other.
Territory Health Minister Natasha Fyles has written to both the Federal Health Minister and Indigenous Health Minister, asking them to help fund a co-ordinated approach to the outbreak.
She says while the NT Health Department and the Aboriginal Community Controlled Health Sector are working together to tackle the NT’s high rates of STIs, they need additional support from the Feds to target remote indigenous populations — which are highly mobile and often cross state boundaries.
But politicians in Canberra maintain the NT’s alarming STI rates aren’t their problem — and that they’ve already coughed up enough to control the scourge.
Indigenous Health Minister Ken Wyatt says the Government has already allocated $8.5 million for the delivery of direct services and support in the Northern Territory.
They’ve also coughed up $8.8 million to address the outbreak of infectious syphilis in indigenous populations in central and Northern Australia, a plan which will see enhanced rapid response kits rolled out across the Territory.
As well as this multi-million cash splash, Mr Wyatt says $21.2 million in funding is also being invested from 2017-2021 through its Aboriginal Community Controlled Health Services in outbreak regions. “State and Territory Governments have constitutional responsibility for providing sexual health services, but the Australian Government also contributes to sexual health funding, recognising the importance of this issue,” Mr Wyatt says.
But Ms Fyles says the Commonwealth’s expanded funding has only been provided Aboriginal Community Controlled Health Services, even though half the primary health care services are provided by the NT Government health centres.
She insists the NT Government is delivering on its role in outbreak control, through the Centre for Disease Control.
It’s not good enough for shadow health minister Lia Finocchiaro, who wants politicians to work together to tackle the issue.
“The high rate of sexually transmitted infections in the Territory is unacceptable and needs a targeted approach,” she says.
“Commonwealth and Territory governments need to work harder to ensure that sufficient funding is delivering outcomes on the ground.”
And still, as the pollies bicker, the NT’s STI rates continue to climb.
ASSOCIATE Professor James Ward has been working with Aboriginal health and communities in Australia for more than 20 years.
He’s a Pitjantjatjara Nurrunga man, and heads South Australian Health and Medical Research Institute’s Infectious Diseases Research Program in Aboriginal Health.
Put simply, Prof Ward wants the NT Government to focus on the basics — to teach Territory school kids more about STIs in the classroom and to invest in aboriginal healthcare workers across remote areas.
“We have a very high turnover of staff that work in remote clinics across the Territory,” he says.
“The median stay of a remote area nurse is four months in remote communities, that impacts on conscience of care and obviously on preventive issues such as STI control.”
Looking at figures over the past 20 years, Prof Ward says the prevalence of STIs in remote NT communities is so high that without additional resources the rates won’t come down.
“I think bolstering the sexual health workforce in the NT would be a very good start,” he says.
Prof Ward says in remote communities, sexual networks are very small so STIs are easily passed around.
“That doesn’t mean everyone in communities has sex with each other, but it’s the interconnectivity of the network that plays into STI prevenance, and sustained for a very long time,” he says.
“Almost every single young person needs to be tested every year.”
But getting people to come in and get tested is hard, considering the shame and stigma around STIs.
Boosting the number of young people getting themselves checked is also a priority for Central Australian Aboriginal Congress chief executive Donna Ah Chee.
“Like other Aboriginal community controlled health services, Congress is extremely concerned about the unacceptable rate of STIs in our communities — especially among young people,” she says.
Congress is helping with a number of new initiatives to help address the Territory’s high STI rates.
One project encourages young people between the ages of 15 and 29 to get STI tests and follow up their appointments by gifting them a $30 phone card.
■ ■ ■
WHILE these programs are encouraged by health professionals across the Territory, Australian Medical Association NT president Rob Parker insists more investment is needed.
Dr Parker says the NT is in the middle of a gonorrhoea and syphilis “epidemic” — infections which are going untreated and easily crossing state lines in remote communities.
Every year, the NT Government spends about $7 million running the Territory’s Centre for Disease Control’s sexual health and blood borne virus — which includes personnel, operational and grants expenses.
Dr Parker wants the Commonwealth to establish a national CDC, which can facilitate a national approach to the problem.
“The problem is it’s not just in the Northern Territory that’s the problem,” he says. “You need an effective co-ordination process.”
Dr Parker says the Federal Government has “failed” in its duty to respond to the national sexual health crisis.
Despite the call, Mr Wyatt is insisting establishing a nation CDC will not “add anything material” to Australia’s capacity to respond to national communicable disease outbreaks.
He’s not committed to increasing any of the NT’s funding, and it’s still a few months before the Gunner Government shows its budget.
Considering its terrible financial status, it’s unlikely to make a massive investment.
Territory CDC section head of the sexual health and blood bourne virus unit Sally Singleton says different Australian jurisdictions do work together to share information.
She’s unsure if a national branch will make much of a difference in tackling the crisis.
Looking at the figures, Dr Singleton admits its clear the NT does have a STI problem, with the whole of the NT now designated as a “syphilis outbreak zone” and high, sustained rates of both gonorrhoea and chlamydia.
However, Dr Singleton says not all the figures are bad.
The sexual health expert doesn’t know if the increase in NT STI rates is, at least in part, owning to a higher number of people being tested.
“There was a really good increase in the number of tests that were being done following the syphilis outbreak,” Dr Singleton says.
“We don't get the data on all the number of tests that are done, we get the results.”
Prof Ward is also happy to see an increase in the number of people getting checked, but says the consequences for STIs are “really understated”.
He says Australian research shows STIs, when left untreated, can mean life or death.
“For women who have been diagnosed with chlamydia and or gonorrhoea, the risk of ectopic pregnancy, pelvic inflammatory disease and infertility is about twice that for aboriginal women than what it is for non Aboriginal women,” he says.
“It’s not only about young people having an STI and the shame and stigma associated with that, it's the morbidity for young women.”
Prof Ward also says when someone has one STI, their chance of getting HIV increases between two and five fold compared to someone exposed to HIV but that doesn’t have a STI. “If HIV became more prevalent across remote Australia we’d be in big trouble,” he says.
The sexual health expert is also worried about the “very real threat” gonorrhoea will be resistant to all treatment in future.
“We need to elevate STIs as a health issue, particularly for young adults,” he says.
“The consequences are too serious if we don’t.”


Add your comment to this story
To join the conversation, please log in. Don't have an account? Register
Join the conversation, you are commenting as Logout
From the Top End to SA: Untold stories shared in new book on railway history
Russians, railways, bridge thefts, and more – one author’s 20-year project on the untold history of the railways between Darwin and Adelaide has hit the shelves of Territory book stores.
Heart of gold: Life on site at Australia’s most remote mine
With the NT News being given unprecedented access to the Territory’s largest gold mine, take a peek behind the scenes – and meet some of the characters who make the mine tick.