RDH emergency department research shows DV victims falling through the cracks
A study of a Top End emergency department has revealed less than 40 per cent of domestic violence patients were seen by a social worker.

Indigenous Affairs
Don't miss out on the headlines from Indigenous Affairs. Followed categories will be added to My News.
A study of presentations to a Top End emergency department has revealed domestic violence patients left before completing their care 10 times more often than others, while less than 40 per cent were seen by a social worker.
The research by Royal Darwin Hospital doctors, led by Dr Lucy Owen, said the findings demonstrated “a failure of service provision” to the patients.
Despite the nine-fold early discharge rate, patients experiencing DV spent twice as long in the emergency department – many told to wait until morning to see social services.
Given most people with DV injuries attended hospital outside of business hours, the researchers said it was crucial all healthcare workers could help fill the gap until social workers were available.
“There is a need for a 24 hour trauma-informed, culturally safe and integrated service,” the study published in Emergency Medicine Australasia said.
“With low rates of engagement with the social work service it is essential that all healthcare professionals are trained in the basics of sensitive inquiry and can make consensual referrals to specialist services.”

Out of more than 6000 patients studied, 1.2 per cent were domestic violence related – a rate five times higher than that of a metropolitan women’s hospital in Queensland.
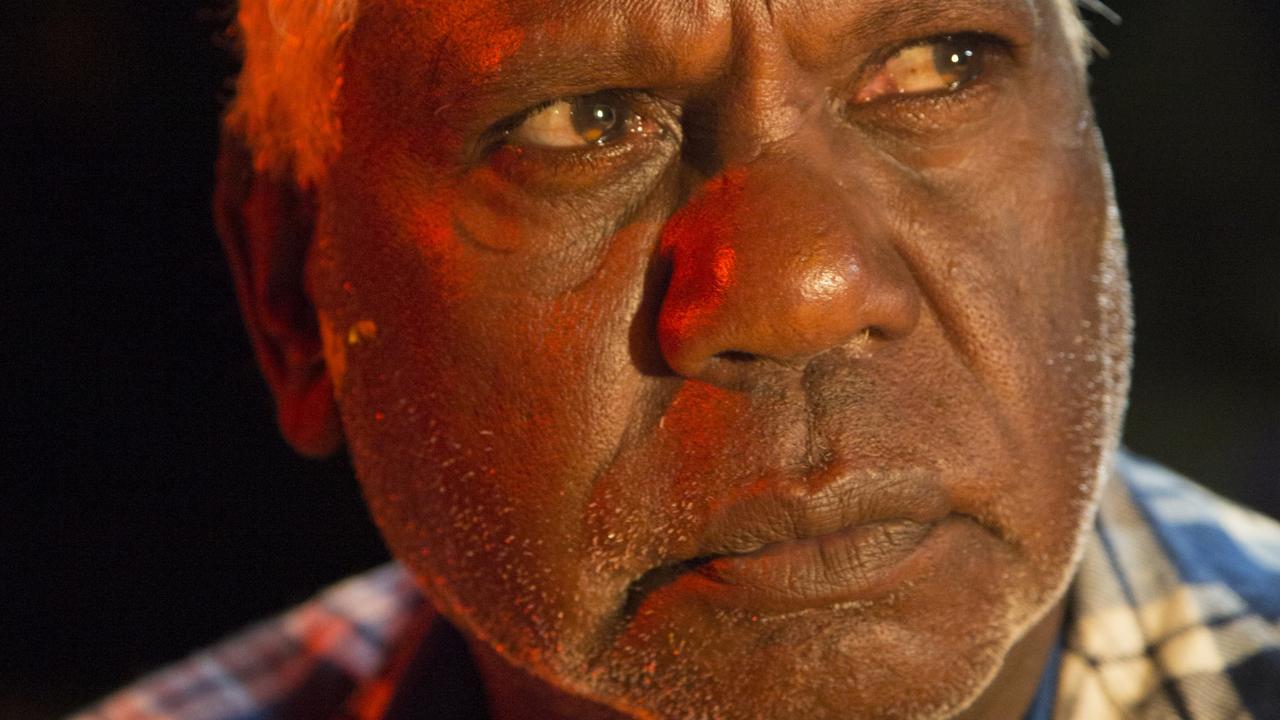
Of the DV patients, 90 per cent were Indigenous, 77.1 per cent were women, and more than two thirds were younger than 40.
Only 37.1 per cent accessed a social worker and a third had been to the emergency department with a DV injury in the past six months.
In comparison, a metropolitan emergency department with a round the clock social work service saw two thirds of DV patients.
Many of the cases were complex – 30 per cent were homeless, just under half were intoxicated, and one in 10 were pregnant – yet more than half of the patients left without a formal risk assessment.
It was noted that RDH was introducing a new process in an attempt to better deal with risky cases – mandating a minimum triage score, streamlining access to the short stay unit and facilitating direct after hours referrals to specialist DV services.