Congress presents solutions to Central Australia healthcare ‘crisis’
The Central Australian Aboriginal Congress has called for changes to visa settings for international doctors to keep remote clinics operational, as the latest stats reveal a huge shift in skilled workers moving to the Red Centre.
Alice Springs
Don't miss out on the headlines from Alice Springs. Followed categories will be added to My News.
The Australian government is considering ways to streamline international healthcare workers to remote settings as health clinics struggle to maintain their workforce.
A spokesman from the Department of Health and Aged Care said the Australian Health Practitioner Regulation Agency was “actioning key actions from an internal review” to reduce bureaucratic red tape and timelines for registration of international health workers.
“Additional work is also being done at the request of National Cabinet,” he said.
It comes as data from the Department of Home Affairs reveals GP visa grants under the Temporary Skill Shortage 482 visa had dropped to 283 in 2021-2022, down from 354 in 2020-2021 and 410 in 2019-2020.

Both departments did not answer questions about how many of these workers had chosen to work in MM2 areas - meaning outer suburban areas of large cities.
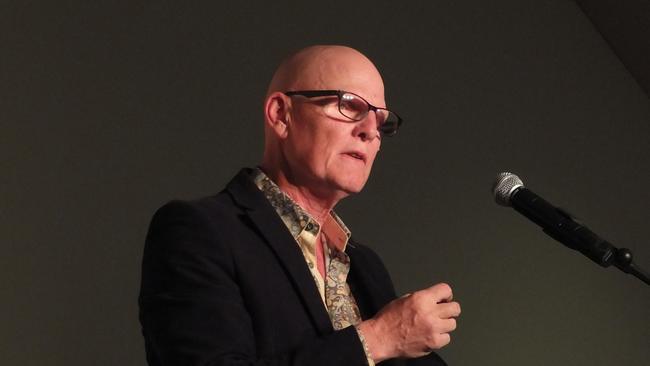
Central Australian Aboriginal Congress chief medical officer Dr John Boffa said MM2 localities needed to once again be made off limits for international medical graduates, or regions would suffer.
Congress presents solutions to Central Australia healthcare ‘crisis’
A critical worker shortage has forced an Alice Springs health clinic to temporarily close, as the Congress demands “urgent” action to bring health workers into remote areas.
Central Australian Aboriginal Congress chief medical officer Dr John Boffa said the primary healthcare worker shortage in rural and remote NT had reached “breaking point”.
“The critical shortage of doctors, nurses, Aboriginal health practitioners, allied health and other staff has forced Congress to temporarily close one of our Alice Springs clinics, as we prioritise keeping our remote clinics open,” he said.
“This situation is unacceptable and urgent action is needed.”
CAAC, known as Congress, runs 14 clinics across remote and rural NT, including the Yulara and Imanpa health clinics which it took over this month.
The Northside Clinic, on the Stuart Highway in Alice Springs, is listed as being closed until April due to “continuing staff shortages”.
If there were no immediate changes, especially to the visa process for international health professionals, it would increasingly struggle to maintain services in remote communities, he said.
Dr Boffa said they were currently short about a third of their staff, meaning they are unable to grant leave to their current staff as they normally would which added pressure to remaining staff.
Dr Boffa said the shortages threatened to undermine an improvement on life expectancy gains in the Northern Territory, where the life expectancy gap between Indigenous and non-Indigenous people is the widest of any state or territory.
“Life expectancy gains have been led by primary health care services such as congress. But this progress is at serious risk of stalling if we do not urgently address the workforce crisis.”
Congress has introduced a number of proposed strategies to help deal with the workforce crisis, including easier access for international health professionals to work in remote regions of the country.
“Australia cannot afford to bring in doctors from overseas and let them work where they are not needed – especially when the needs in remote areas are so great,” Dr Boffa said.
“Address these needs by making MM2 localities off limits for international medical graduates and non-vocationally registered Australian doctors; or watch these doctors continue to leave areas of need and go and work in capital cities.”
Other short term strategies proposed by the CAAC included retention payments for remote nurses after 12 months of work, a national campaign encouraging practitioners to return regularly to communities over a number of years, and an increase in the Medicare bulk billing incentive in rural and remote areas to match the “large increase” in the cost of employing health professionals in those communities.
It comes as St John NT launches a recruitment drive to the United Kingdom and New Zealand, following two remote stations being 80 per cent short on staff.




