Coronavirus vaccine: French government demands equal access in COVID-19 vaccine distribution row
A simple comment from the boss of a pharmaceutical company this week has sparked a glimpse of how ugly the battle for a vaccine could get. So who is first in line?
The first shot in a potential war over access to a COVID-19 vaccine has been fired in France after a stoush between a pharmaceutical CEO and politicians.
Drug giant Sanofi’s CEO Paul Hudson sparked anger this week when he said the US government had first rights to a pre-order of a vaccine in development because “it’s invested in taking the risk.”
The move was swiftly shot down by French Prime Minister Edouard Philippe who said a vaccine should be a “public good for the world” and that “equal access” was “non-negotiable”.
Comme l’a indiqué @EmmanuelMacron, un vaccin contre le #COVID19 devra être un bien public mondial. L’égal accès de tous au vaccin n’est pas négociable.
— Edouard Philippe (@EPhilippePM) May 14, 2020
US Secretary of State Mike Pompeo was drawn in and said he hoped any vaccine development would be shared around the world.
“I hope that we will all collectively find a way to produce this at high volume to get it all across the world and make sure that every citizen that needs access to a vaccine can get it as quickly as possible.”
Meanwhile Mr Hudson apologised and will meet French President Emmanuel Macron to discuss the issue next week.
MORE: Follow the latest virus news here
MORE: PM proposes date for return of travel
But whether Hudson’s comments were simply clumsily worded or a harbinger of what’s to come in the face for a COVID-19 vaccine remains to be seen.
The World Health Organisation (WHO) regards finding an effective vaccination as a “moon shot” that won’t necessarily mean the virus will be eradicated, according to comments made this week by Dr Michael Ryan.
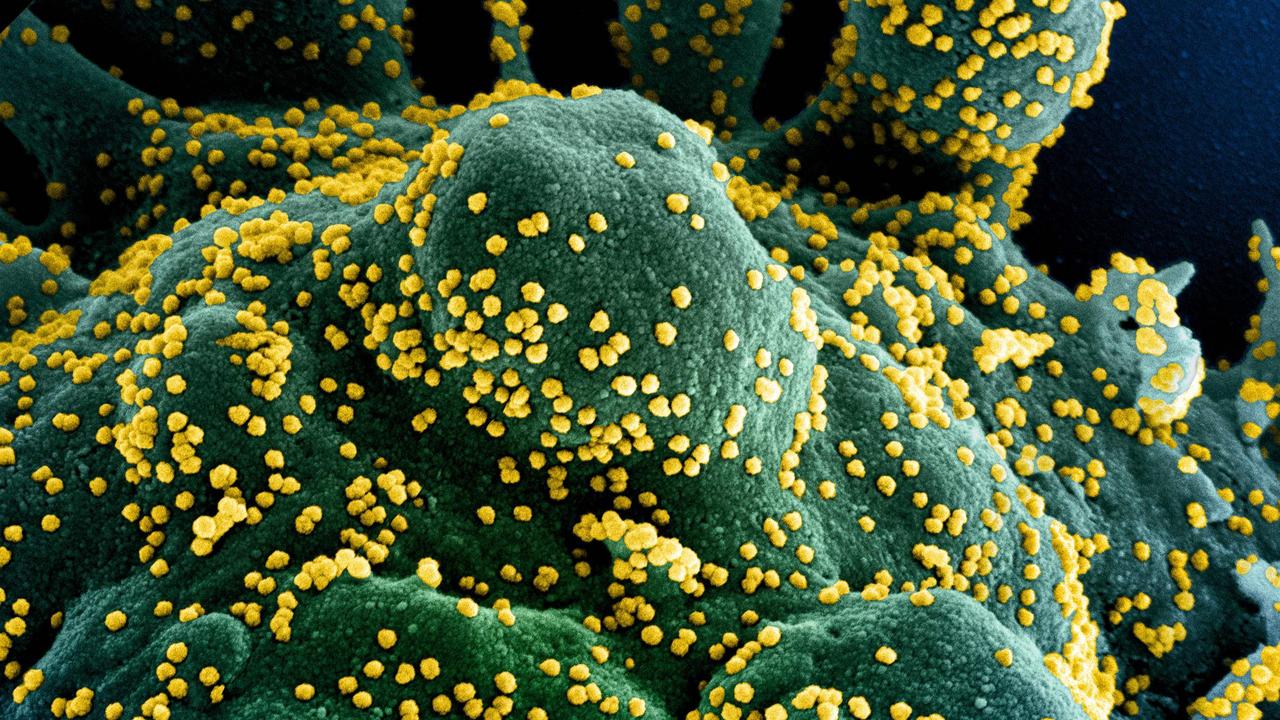
So far more than 90 potential vaccines are in development around the world with eight in the human trial stage.

The University of Oxford’s Jenner Institute is currently leading the race with a vaccine derived from a chimpanzee virus already in human trials and preliminary results expected within two to six months. The researchers have announced a partnership with pharmaceutical company AstraZeneca that would see both partners operate on a not-for-profit basis during the course of the pandemic.
Comments hailing the partnership including include references to the “British people” that may also provide clues as to how it will be distributed.
Oxford University’s Vice Chancellor Professor Louise Richardson said if successful, the partnership will “ensure that the British people and people across the world, especially in low and middle income countries, will be protected from this terrible virus as quickly as possible.”
UK Health Secretary Matt Hancock also said a vaccine is the “best hope of defeating this virus for good”.
“I am determined to do everything in my power to develop an effective vaccine and get it to the people of the UK as soon as possible. I want the UK to lead the world in developing a coronavirus vaccine – and I will back our scientists to the hilt in doing so,” he said.

‘BIG LEAP’ FROM TRIALS TO REALITY
Charlie Weller, the head of vaccines at London-based medical research charity The Wellcome Trust, said she’s “optimistic” about the prospects of a vaccine being developed but “there really are no guarantees.”
She said the pandemic has created enormous challenges that have never been seen in our lifetime with a “big leap” to be made from proving a vaccine effective to having it available for global distribution.
“We’ve never had the challenge we’ve had today in anyone’s lifetime. We’re looking to develop a vaccine within a year. Normally it takes ten years. Then we’re trying to have it available for everyone in the world. Everyone will be wanting this vaccine and needing this vaccine at the same time,” she told news.com.au.
“I am optimistic … but even if that’s possible, it’s likely in that first year that there won’t be sufficient doses and decisions will need to be made on who gets that initial healthcare allocation.”
The organisation is one of several healthcare giants along with the WHO, Bill and Melinda Gates Foundation, International Red Cross and leaders of France, South Africa, Germany, Italy, UK and others to launch the ACT Accelerator that will help define the criteria for priority candidates and ensure equitable global distribution of vaccines and treatments for the virus.
It comes after recent experiences with HIV and the H1N1 bird flu outbreak in 2009 where treatments were available but not used effectively. WHO Director General Dr Tedros Adhanom Ghebreyesus has always insisted global solidarity is key to beating the virus.
Ms Weller didn’t rule out the process becoming political, but said vaccine manufacture and distribution is not as black and white as one might think.
“We don’t know where a vaccine is coming from. If each country decides to focus on its own national interests and then if that country is not able to develop a vaccine then what happens? The only viable route forward for everyone to have access is to have a co-ordinated global system.


THINK GLOBAL, ACT LOCAL?
Assuming an effective vaccine can be found, it will inevitably lead to questions over who should be given priority access. In the case of COVID-19, this takes on an international dimension. Do we prioritise healthcare workers and the elderly before young people, who are least likely to fall seriously ill? Or should it be given to young people who can get back to work and get the economy moving? What about international healthcare workers versus a general population?
Oxford University’s senior research fellow at the Centre for Practical Ethics, Alberto Giubilini, is also of the opinion that tough decisions will need to be made and said those could depend on the characteristics of the vaccine itself.
“In the case of the flu vaccine, the evidence suggests it’s easier to build up immunity at a collective level if you target children. That’s not the policy countries follow, but that’s what the evidence suggests,” he said, having produced a research paper on the subject.
“If children get flu they’re likely to be OK, but if you vaccinate children they’re more likely to build up immunity to protect the elderly. There might be a case for prioritising children even if they are the ones who don’t get it more severely, but that depends a lot on characteristics of the vaccine. We do not know at the moment.”
Despite a small but vocal cohort of anti-vaxxers and conspiracy theorists, he also believes a vaccine should be compulsory, at least for certain groups.
“That’s the most effective way to build up immunity. Considering how big of a cost everyone is paying at the moment in terms of economics, liberty, mental health. It’s fair that everyone makes a contribution to get everyone out.”