Coronavirus ‘mutant’ strain six times worse, scientists find
The worst fears of epidemiologists have been realised: COVID-19 has mutated – and this super strain now dominating the world.

The worst fears of epidemiologists have been realised: COVID-19 has mutated, and the strain now dominating the world is up to six times more infectious.
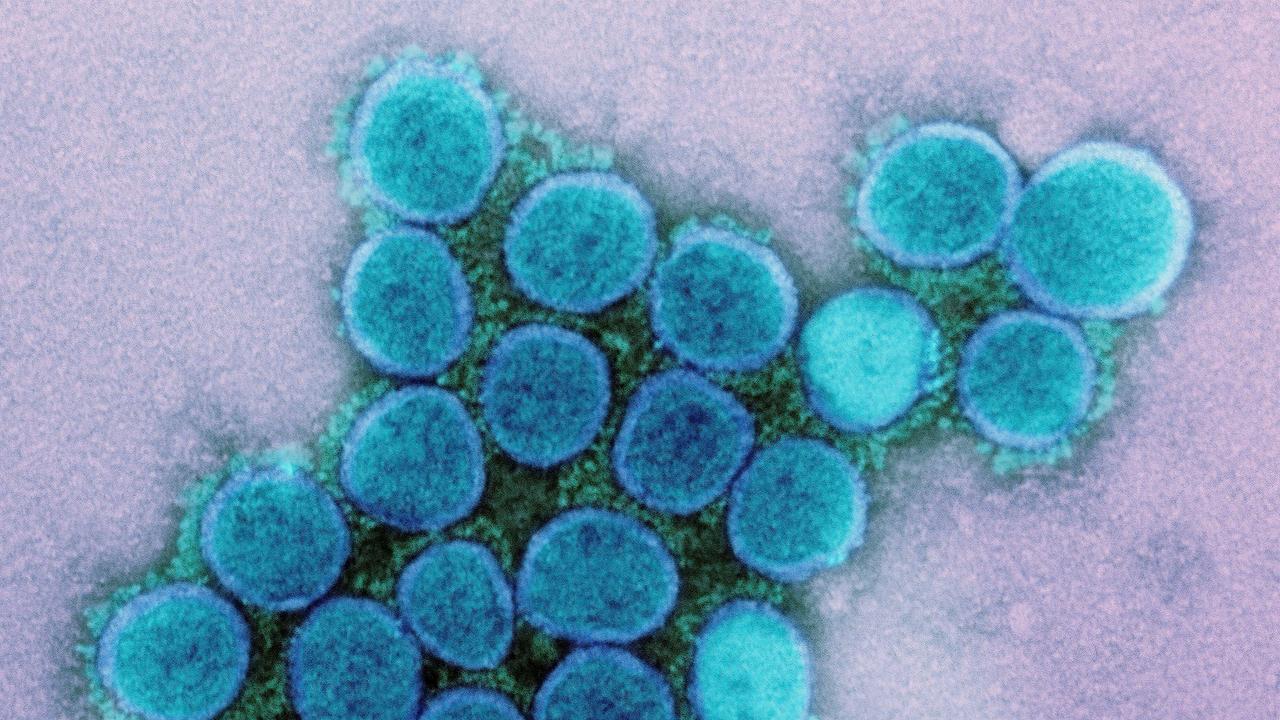
New research published in the science journal Cell cites laboratory research as identifying small changes in the proteins that protrude from the surface of the COVID-19 virus. These changes, which have evolved during the past six months, enhance its abilities to jump between humans – but have not increased or reduced its symptoms.
The public face of the United States’ fight against the exploding pandemic, Dr Anthony Fauci, told the American Medical Association at the weekend the findings – while unconfirmed – could be significant.
“I think the data is showing that there is a single mutation that actually makes the virus be able to replicate better, and maybe have high viral loads,” he said.
Viral load refers to the amount of virus colonising a sufferer.
RELATED: ‘Monstrous’: US in virus ‘freefall’

The study was conducted by the Los Alamos National Laboratory in New Mexico, the Duke University in North Carolina and the University of Sheffield’s COVID-19 Genomics UK research group.
The team studied 999 British patients being treated for severe infections, as well as conducting laboratory experiments on how effective the virus was at breaching the defences of human cells.
The researchers revisited their initial work in June after the scientific peer-review process challenged the extent of their findings. The revised results indicate the current strain – D614G – is between three and six times more infectious than the original first detected in the Chinese city of Wuhan.
But exactly how this mutated protein affects the transmission of COVID-19 outside of a laboratory environment is yet to be determined.
“We don’t have a connection to whether an individual does worse with this (strain) or not,” Dr Fauci says. “It just seems that the virus replicates better and may be more transmissible.”
IMMUNITY UNCERTAIN
Hopes for a successful vaccination remain high. But the chances of populations suffering through a COVID-19 outbreak emerging with a degree of “herd immunity” have been dealt a serious blow.
A series of new studies suggest that our immune systems are so strained fighting the coronavirus that it isn’t producing enough antibodies to resist reinfection longer than a few weeks or months.
RELATED: Why US is facing 100,000 cases a day

One recent paper published by Nature Medicine concludes the hope that those who have recovered cannot again contract and spread the virus – and therefore choke the spread of the pandemic – appears unfounded. Asymptomatic carriers, in particular, appear to emerge from infection with no detectable antibody levels at all.
But the concept of herd immunity is not dead and buried.
Vaccination is hoped to produce effective levels of long-lasting antibodies. But such a vaccination remains some considerable time off. And then there is the human body’s other method of fighting off infection: T-cell memory.
“Most people are generally not aware of T cell immunity, and so much of the conversation has focused on antibody levels,” Columbia University virologist Angela Rasmussen told the New York Times.
These cells learn from past infections. They can react to the discovery of a known infection by manufacturing in bulk the antibodies it already knows can defeat it.
More than 60 per cent of a population needs immunity from infection for the concept of herd immunity to reduce the opportunity of a disease to spread to the point where it “burns out”.
A WEIRD VIRUS
COVID-19 isn’t behaving as expected. It’s a respiratory illness: so coughs, fever and a shortness of breath is to be expected. But blue toes? Heart attacks? Blood in faeces? A loss of smell? Exactly why some patients show these symptoms and not others is unclear. But we know it’s happening.
RELATED: ‘Clear failure’: Truth about Vic clusters
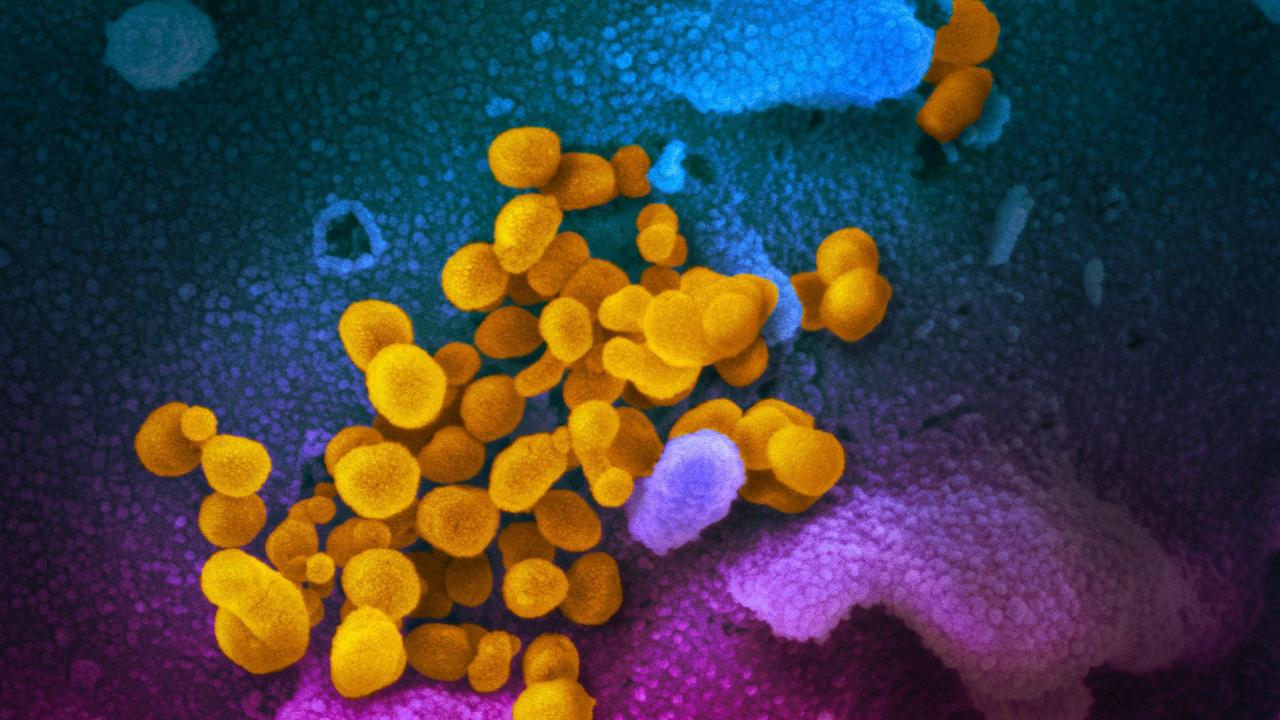
It’s all related to a specific protein receptor. Such receptors cover cells. They receive chemical “keys” from the body to turn on or off specific functions. One such “lock” – ACE2 – is found on many different kinds of human cells across the body.
And COVID-19 has a copy of the ACE2 protein “key”. And once COVID-19 breaks into a cell, it’s dead.
Cells with ACE2 receptors can be found in the nasal passage in an area associated with smell. But it’s also in some lung, heart, kidney, liver, gastrointestinal and blood vessel cells.
We’re not certain how the virus gets to these vital organs in some people, but not others.
But research suggests our immune systems are not helping. It can overreact. It can fight back so hard, it can cause intense inflammation.
In severe cases, the immune system ends up damaging the same lungs, kidneys, heart – and the smallest of blood vessels, such as those found in toes – it’s supposed to protect.
Virologists say this is not entirely unusual. Other viruses can also trigger overreactions, such as influenza and brain swelling. What is unusual is COVID-19 itself. It’s new. It’s nasty. And we’re not yet certain of how it works.
Jamie Seidel is a freelance writer | @JamieSeidel