Australia Covid: Epidemiologist exposes big issue with states’ Covid numbers
There is a big difference in one key Covid measure between different states, and it is leaving Australia to “shoot in the dark”, experts say.

Despite being two-and-a-half years of daily pandemic updates, mortality rates and a growing vocabulary of epidemiology, there are still situations in Australia’s Covid response that aren’t up to scratch, says a top virus expert.
Deakin University’s chair in epidemiology Catherine Bennett says the issue can be seen in the stark difference in hospitalisation figures between NSW and Victoria. On Friday, NSW (with a population of 8.1 million) reported 2257 hospitalisations, while Victoria (with a population of 6.6 million) reported 813.
A key reason for the difference lies in the fact that hospitalisations due to Covid are assessed on different criteria in different states.
A spokesperson from NSW Health confirmed to news.com.au that the state’s hospitalisation figures cover all patients who have tested positive for Covid-19, regardless of why they were admitted. This could cover someone who tests positive and experiences a mild case of Covid while undergoing treatment for a broken arm.
They will then continue to be counted in the hospitalisation figure until they are discharged, regardless of whether they have cleared the virus before this date.
COVID-19 update – Friday 29 July 2022
— NSW Health (@NSWHealth) July 28, 2022
In the 24-hour reporting period to 4pm yesterday:
- 96.8% of people aged 16+ have had one dose of a COVID-19 vaccine*
- 95.3% of people aged 16+ have had two doses of a COVID-19 vaccine* pic.twitter.com/W7We68rBZs
In Victoria, however, the hospitalisation figure only relates to people who are actively testing positive to Covid. This means a patient is removed from the daily hospitalisation figure once they are no longer testing positive to Covid.
In a statement to news.com.au, Victorian Department of Health (DHHS) confirmed that the state’s “Covid-19 hospitalisations (are) based on confirmed COVID-19 positive patients currently occupying an admitted bed, including ED short stay unit, ICU, acute same-day, acute multiday and overnight, and mental health.”
“[Victoria] seem to cut it short,” says Prof Bennett.
“Even if you did go in there for Covid and you’re there for a month, you’re only counted for the time you’re infectious.
“I don’t know how they do that but [their numbers] seem to be very low compared to other states.”

The inconsistencies make it difficult to determine the impact of Covid on the hospital system, and therefore what would be the most helpful solution to alleviate that, says Prof Bennett.
Prof Bennett makes the point that a lack of data around hospitalisations means we’re unable to properly assess the impact of Covid.
She believes there needs to be a lot more research on how many more people are getting admitted to hospital due to severe Covid, something which the figures around hospitalisations don’t actually convey.
“Are the main counts in hospital now because people are there for other reasons or is it excess hospitalisations because of Covid?
“We’re not getting that data. No one’s reporting that,” she says.
“We know that hospitals are stressed. A longer flu season, the extra Covid cases and an impacted workforce is going to give you that stressful situation but we don’t know how much of that is driven by people with severe illness from Covid.”
‘Shooting in the dark’
The leading epidemiologist says that aspects of Australia’s systems and processes around capturing Covid data and the reporting of severe Covid have left us “shooting in the dark” – especially during a winter which we “knew was going to be tough”.
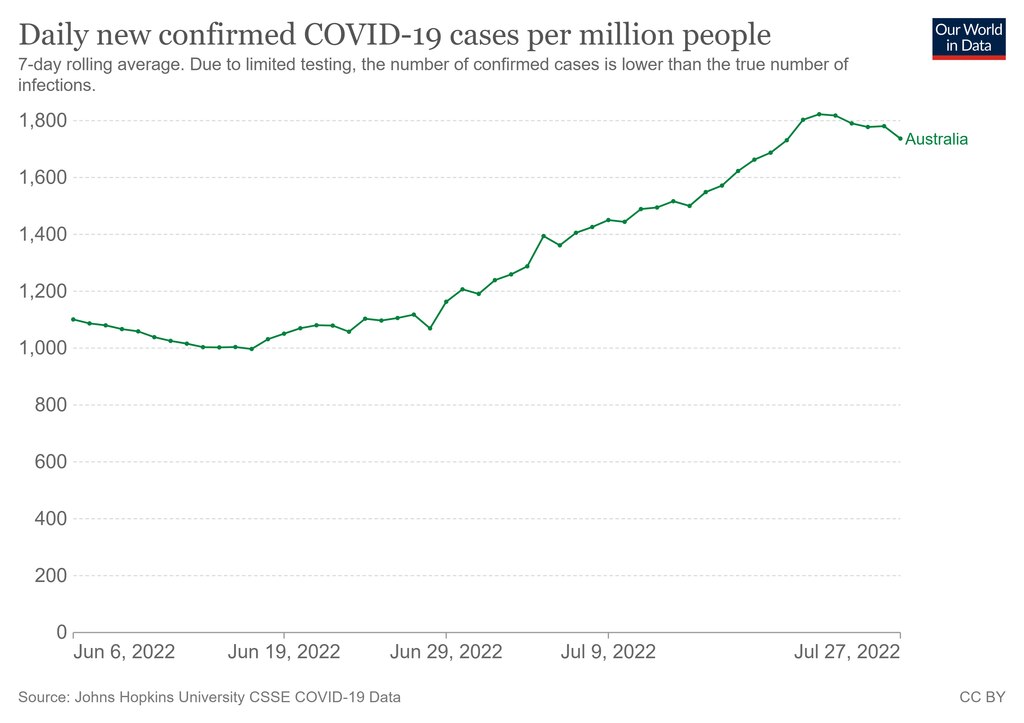
This comes as Australia battles through another “very, very significant” Omicron wave, as the more infectious BA.4 and BA.5 sub-variants take hold.
According to updates from the Department of Health and Aged Care, cases have increased across the country, with hospitalisations and deaths also on the rise.
Earlier this month, chief medical officer Paul Kelly and Health Minister Mark Butler urged people to practice good hand hygiene and physical distancing, in advice that Australians have heard many times before. Without resorting to strict mandates, Prof Kelly encouraged people to wear masks in the workplace, or better yet, work from home.
“This third Omicron wave for 2022 is proving to be a very, very significant one,’’ Mr Butler said. “There were 300,000 cases or thereabouts reported over the last seven days, and I think the CMO and I are pretty confident that the real number is likely to be more than double that.
“We are seeing hundreds and hundreds of thousands of Australians infected every single week in this wave. As of today, there are more than 5200 Australians in hospital with Covid. That number has increased very dramatically over recent weeks.”

‘We could do it in a week’
In Prof Bennett’s opinion, a lack of accurate data also means people are unable to “understand the risk and therefore how to manage it”.
This includes information and increased “surveillance” on the mix of variants currently circulating, and infection on the basis of gender, age, locality and occupation. This is particularly important given the fact that current Covid figures are most likely only capturing 50 per cent of actual cases, Prof Bennett says.
“At the moment, we’re getting a snapshot of the variants causing severe infection at the hospital end but that doesn’t reflect what’s happening in the general population.”

However, she believes this is an issue that could be corrected in a week. The data could then be used to inform improved pandemic modelling, which now needs to incorporate multiple variants, sub-variants and issues like reinfection and immune escape.
“It would be an investment, but we could do it this week and we could have the information we need, in order to decide by the end of the week,” she says.
“Why would you be doing modelling if you’re not collecting the data to inform the modellers? Modelling depends on really accurate parameters.”
Blurring lines between Covid, the flu and a cold
The increase of colds and flu in the community has also continued to cause a polarised response to Covid, which further exacerbates the issue. This is also in part due to the different symptoms associated with the BA.4 and BA.5 Omicron variants which have resulted in light headaches and more mild cold-like symptoms.
“Winter flu and the cold might give some people an out because they think it’s nothing, but for other people, every sniffle is Covid. They think it’s terrible and it’s going to kill them,” she says.
“The muddling of different infections in winter is, if anything, contributing to the polarisation.
“But if everyone is in the middle and being careful and restricting their movements, then we would probably travel through this a bit better.”

This comes as a recent UK public health study from the health app Zoe found that the most common Covid symptoms were now a cough, hoarse voice, sneezing, fatigue and muscle aches. This is in comparison to earlier symptoms like fever and a loss of taste and smell, reports The Strait Times.
In response, the lead scientist for the study, Dr Tim Spector, said: “If you have any cold-like symptoms at the moment, it is nearly twice as likely to be Covid-19 than a cold.”
Responding to these claims, Professor Bruce Thompson, head of the Melbourne School of Health Sciences at the University of Melbourne, says the assertion was “not unreasonable”.
“At the moment [the new variants are] way more contagious than the other bugs,” he told news.com.au.
“At the end of the day, coronavirus, is the umbrella term, which includes the common cold.”
However, the reality is that measures which protect against Covid infection, also prevent the transmission of the common cold and flu.
“A lot of the things we are encouraging – including wearing masks – also work against these respiratory infections,” Prof Bennett says.
“If you distance from other people, practice hygiene and wear a mask, you’re less likely to get the cold, flu and Covid.”






