UK baby born with three people’s DNA with pioneering technique mitochondrial donation treatment
One of the first babies created from three genetic parents has been born with pioneernig technology.
The first UK baby created from three genetic parents has been born with pioneernig technology.
Most of the DNA of the baby comes from their two parents but around 0.1 per cent from a third, donor woman.
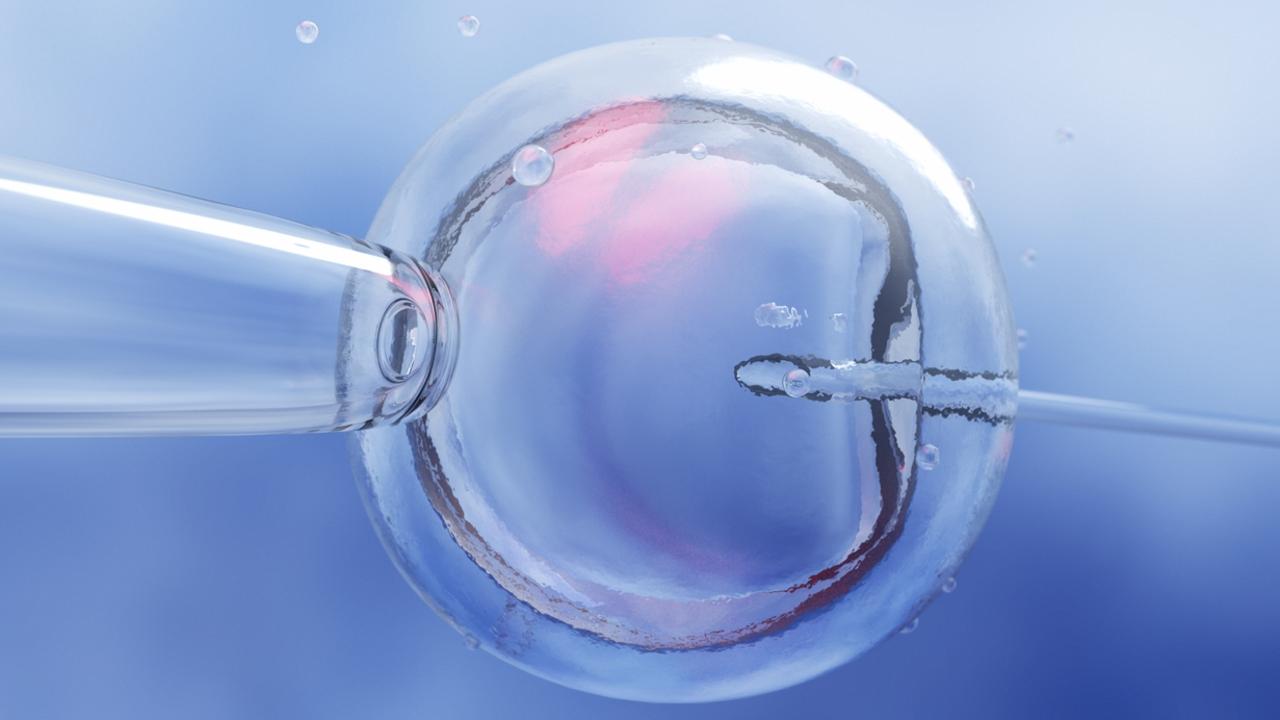
The pioneering technique is known as mitochondrial donation treatment (MDT) and the procedure aims at stopping a mother from passing on defective genes in the mitochondria – tiny power plants in cells that supply energy – to her child.
Nuclear DNA was given to the child from the mother and father, which define key characteristics such as personality and eye colour.

They were also given a tiny amount of mitochondrial DNA provided by the “third parent”.
The breakthrough in the UK was first reported in The Guardian with laws introduced in the UK in 2015 for the creation of such a baby.
Mitochondrial diseases are incurable and can be fatal within days or even hours of birth.
Some families have lost multiple children and this technique is seen as the only option for them to have a healthy child of their own.
Doctors at the clinic in Newcastle — in England’s north-east — where the breakthrough baby was born have not released details of birth from the MDT program.
Recent research has found that in some cases, a tiny number of abnormal mitochondria that are inevitably carried over from the mother’s egg to the donor egg can multiple when the baby is in the womb.

So-called reversion or reversal could lead to a disease in the child.
The UK is not the first country to create babies from MDT.
In 2016, a US doctor announced the world’s first MDT birth after treating a Jordanian woman who carried mitochondrial mutations that cause a fatal condition called Leigh syndrome.
Prior to the treatment performed in Mexico the woman had four miscarriages.
Dagan Wells, a professor of reproductive genetics at the University of Oxford who took part in the UK breakthrough told The Guardian that the clinical experience with MRT was “encouraging” but the number of reported cases “far too small” to draw any definitive conclusions about the “safety or efficacy”.
“Long-term follow-up of the children born is essential,” he said.
“The stage of development when reversal happens is unclear, but it probably occurs at a very early stage. This means that prenatal testing, carried out at about 12 weeks of pregnancy, may well succeed in identifying if reversal has occurred.”
carla.mascarenhas@news.com.au






