Experts send new warnings as they reveal how Covid-19 is still spreading
Experts are sending new warnings surrounding Covid-19 as researchers learn compelling new details about the virus and bust the big myths.

Experts are sending new warnings surrounding Covid-19 as researchers learn compelling new details about the virus and bust the big myths.
Despite appearances, experts say we still face a precarious time ahead as the seasons change, restrictions ease and isolation and overseas arrival testing rules are scrapped, with evidence that shows the methods in which the virus manages to lurk and linger.
They warn new variants are still to come and urge people not to simply brush the virus off as a “cold”, as many of the spaces we inhabit – offices, clubs, gyms, restaurants, schools – fail to make any meaningful change to stop similar events in the future.
With higher case numbers and Australia’s Covid-19 2022 death toll already more than double the number from the previous two years, they say we are at a heightened risk now more than ever as the key components to catching the virus are relatively ignored.
“It is more now than it used to be before because restrictions were removed, no government organisation has improved ventilation, masks are removed, people pretend that nothing is happening,” Polish-Australian physicist and Professor Lidia Morawska explained to news.com.au.
“Infection rates are much higher than they used to be. Some people say Covid is like a cold. Well, people don’t die from colds.
“Look at the number of deaths, are there reports that ten people died because of the cold? People don’t really die because of the cold, but people die daily because of Covid.
“Fifty people dying daily at any other time during the pandemic that would be the end of the world.”
And with the virus’ favourite playtime – winter – approaching and more and more focus on individual responsibility, Professor Morawska warns “this is just the tip of the iceberg”.
Be aware of your surroundings
Professor Morawska knows all too well about the importance of air quality, from pollution to infectious particles, she’s seen it all.
She is so aware, she even carries a device which measures it for her: an Aranet4.
In simple terms, the device measures the amount of carbon dioxide in the air. The higher the concentration of carbon dioxide, the less air flow in the room, therefore the higher the risk.
She carries it wherever she goes; restaurants, cafes, meetings, anywhere big or small.
“If the concentrations are high then I definitely won’t sit there,” Morawska explains.
“If I sit inside it’s often difficult to assess the situation. Airconditioning turns air around but doesn’t bring fresh air,” she explains.
Understanding how the respiratory tract generates infectious particles, how our lungs spew them out and into the air has been a critical task for researchers.
In 2003, while working as a physicist at the Queensland University of Technology (QUT) studying the effects of inhaling fine particles of pollution, Professor Morawska was asked to join a group in Hong Kong by the World Health Organisation (WHO) to help understand the SARS virus that at the time was beginning its deadly spread in the city. To this day, she still works as a Professor in the School of Earth and Atmospheric Sciences at the university and has been actively working with WHO since 1990.
Professor Morawska’s work was notably important because what she found was compelling, “gamechanging” stuff.
Size matters
Covid-19 has many similarities to its older coronavirus cousin, SARS.
SARS is a viral respiratory disease that was first identified in Southern China in November, 2002. By February, 2003, it was in Hong Kong where it began to spread rapidly.
It is airborne and similarly spreads through tiny respiratory drops, or aerosols.
It struck four countries and according to WHO “was the first severe and readily transmissible new disease to emerge in the 21st century and showed a clear capacity to spread along the routes of international air travel”. It killed about one in 10 infected people.
While the medical community knew the mouth and nose were responsible for expelling infectious particles, what they missed was the size and importance of those infected particles.
Professor Morawska explained that the common belief was that infectious, “very big droplets” would be expressed from our respiratory tracts but due to the nature of their size were not in fact airborne or a higher risk.
“If you have a big particle, sometimes when you’re talking to someone, they get over excited and then you see spit particles come out of their mouth, but these particles don’t go very far because they’re heavy and they drop to the ground,” she said.
“So if it immediately drops down there’s no problem, it’s not in the air. But it was very clear, based on what I learned from our research, that there are very few of these big things and the majority are very small particles which stay in the air.
“Changing the game was to look at the numbers in the air and not just in the immediate vicinity. When people say they’re falling on the ground the reality is the majority of the particles float in the air. That’s the problem with the small particles, the majority will just float.”
What will infect you
Thanks to scientists like Professor Morawska and Trish Greenhalgh, a Professor of Primary Care at the University of Oxford, we know much more now than when we did in 2003.
Professor Greenhalgh’s research, Quantifying transmission risk of SARS-CoV-2 in different situations, noted that the “Omicron variant shows faster transmission and greater vaccine escape than previous variants”. She and her team developed an interactive risk calculator for SARS-CoV-2 transmission incorporating multiple variables including indoors versus outdoors (and level of ventilation if indoors).
Now, we know the virus is in fact airborne. We know some people generate more particles in their respiratory tract than others. That the virus changes location depending on the stage of the disease. And the type of respiratory activity alters how much you omit.
Simple actions like breathing, speaking, singing, coughing and sneezing generate droplets and aerosols of varying size, concentration and viral load.
While we can’t see it, our mouth and our nose are constantly emitting particles which then generates a “plume” around us.
“It’s tiny particles suspended in the air that infect you,” Professor Greenhalgh told news.com.au.
“The thinking nowadays is that the inside surface area of the lung (which is large – the size of a tennis court) is continually exposed over hours or minutes to viral-laden air, and it’s this accumulation over time that constitutes the main risk of becoming infected.
“So we need to move right away from the ‘single ballistic strike’ model.”
Simply breathing creates less particles, but when we speak or sing, we produce a lot. Whether we are infected or not, we are constantly producing. And all of that production has nowhere to go but to float into the air.
“When exhaling there’s continually a blow of particles coming out,” Professor Morawska explains.
“There is lots of liquid there and the air is going at quite a high speed over the surfaces in the respiratory tract”.
The “plume” rises due to the heat of our bodies. Being smaller, the particles are light and stay suspended in the air for a long time. The approximate falling time of a small respiratory particle is 7000 seconds.

How to prove it
Research continues to prove how this type of transmission is the main form of infection for a number of illnesses, Covid-19 included. Research from a number of experts from the National Institute of Allergy and Infectious Diseases in the US earlier this year said epidemiological data confirmed “fine aerosols remain suspended for longer periods and can penetrate all the way down into the alveolar space of the human respiratory tract (lungs)”.
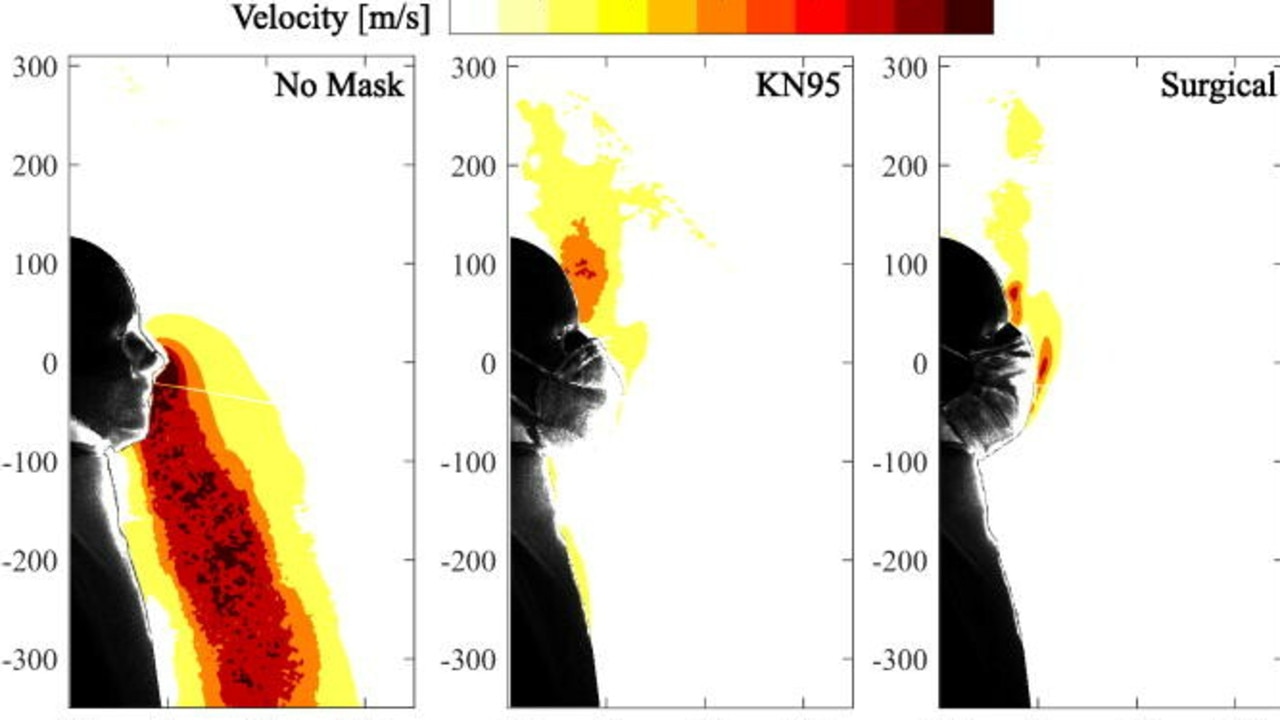
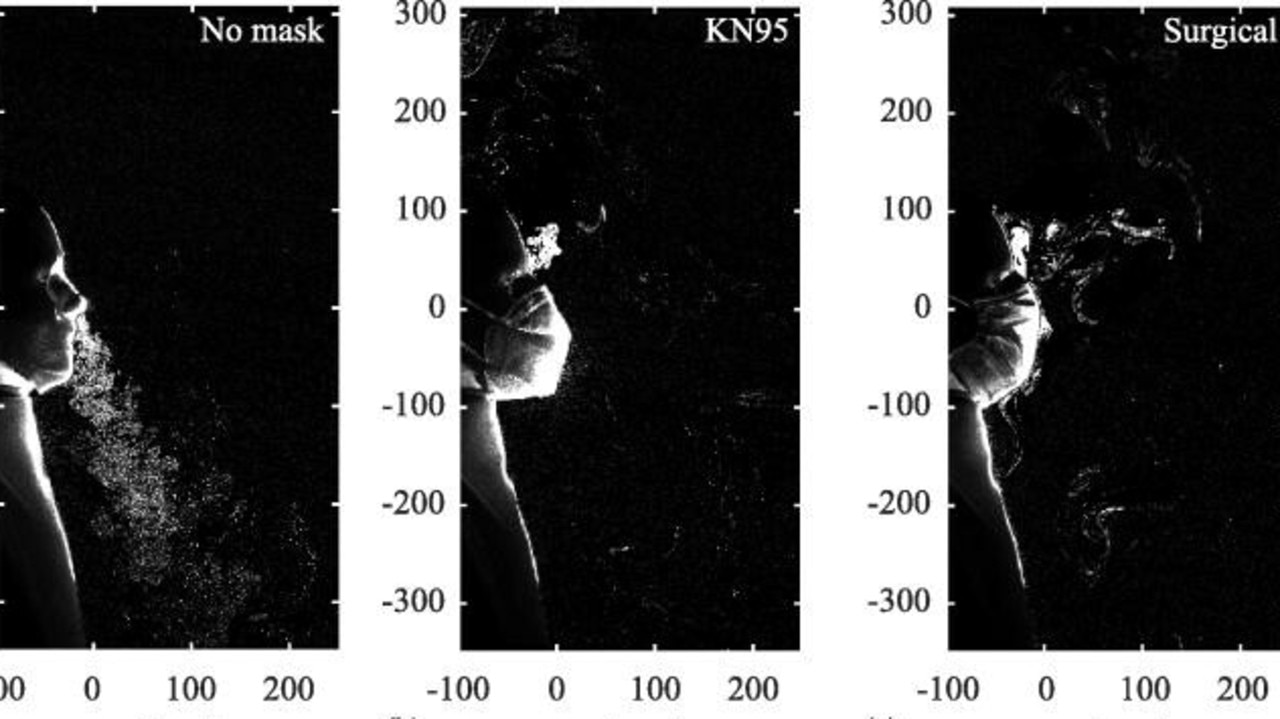
A compelling experiment performed by engineering researchers at the University of Waterloo in Canada created a spectacular visualisation using a mannequin to simulate a seated person breathing in a large room. The study, released last year, showed a significant build-up over time of aerosol droplets, noting: “When not fitted with a mask, exhalation from the nose produces a relatively strong turbulent jet containing well mixed particles that will disperse relatively quickly away from the subject”.
Higher-quality, more expensive N95 and KN95 masks versus cloth and surgical masks filtered more than 50 per cent of the exhaled aerosols that can accumulate indoors and spread the virus when inhaled by other people, it found.
They found that even “modest ventilation rates” were found to be as effective as the best masks in reducing the risk of transmission.
Serhiy Yarusevych, a professor of mechanical and mechatronics engineering and the leader of the study, said the evidence shows that high-quality masks and proper ventilation should be used in combination to mitigate the threat posed by indoor aerosol accumulation as much as possible.
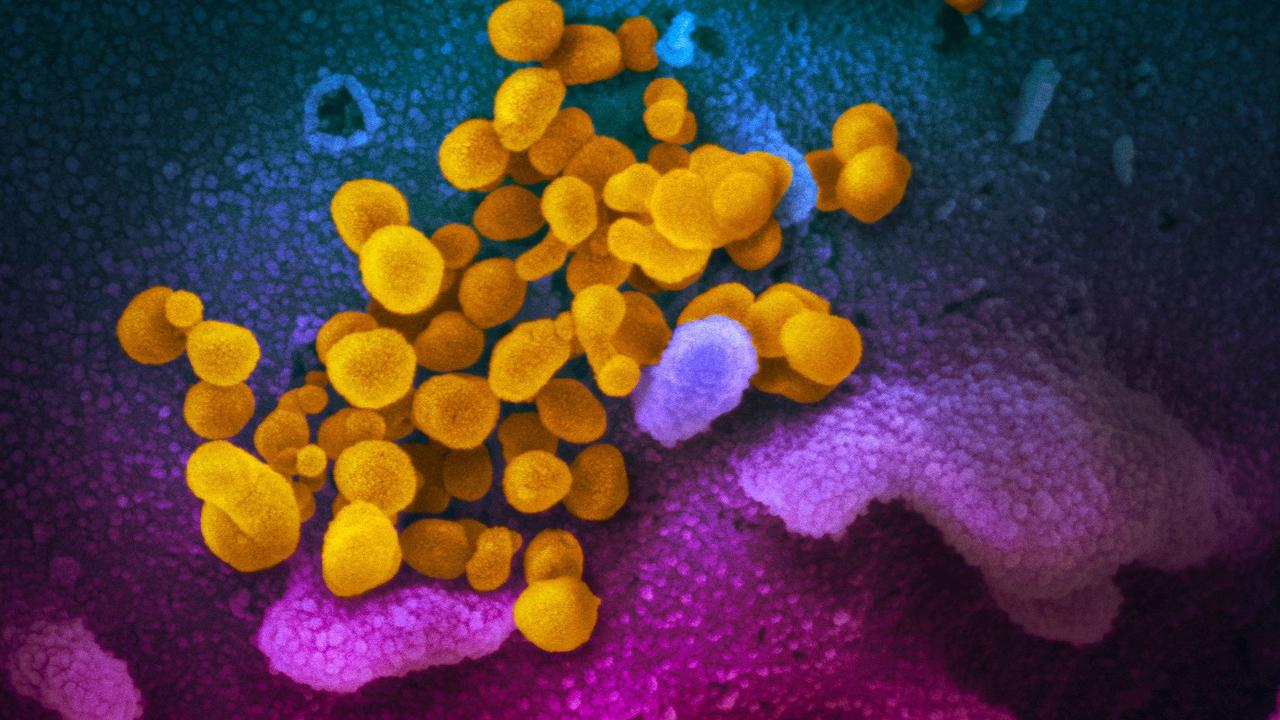
How the virus grows
Covid-19 particularly likes dry and cold conditions, which means dry air. A temperature of below 20, like sometimes in over airconditioned buildings, “is perfect for the virus”. Particularly key components for super spreader events.
Professor Morawska says it can be fairly easy to create a super spreader events if all the elements are “supported”.
“Let’s say it’s a small venue, not well ventilated, with a large number of people, an infected person and all of them standing together,” she explains.
“This is a super spreader event.
“Therefore if you go to a restaurant which has windows closed, no ventilation, we are spending, say two hours having dinner, there’s an infected person there so it has the potential to be a super spreading event.
“The issue is if we are too close to each other, like you are sitting next to another person, this distance of half a meter, even if ventilation is good, you are still in the immediate concentrated plume of initial spray from that person.
“Of course it doesn’t mean that no places are properly ventilated, but in many venues we simply don’t know, whether cinema is ventilated properly or not, we don’t know.”
Those views are backed by other leading experts across the world.
“Yes superspreading events are still possible,” Professor Greenhalgh told news.com.au.
“The dangers of all the different venues relative to one another are still the same but the absolute risk is going to be slightly lower as people get vaccinated and recover from the virus except that a) protection from vaccines wanes over time and b) the virus mutates (vaccine escape).
“So we should not assume anyone is safe.”
Protective measures
Professor Morawska says Australia has all but forgotten the key element of ventilation in states like Queensland and New South Wales, but Victoria has made some progress.
In Queensland the government, “can’t even pronounce the word ‘ventilation’”, she said, while claiming she was “really impressed” how the Victorian government is “taking it seriously”.
Professor Morawska says she is not urging for a “complete lockdown” but made a case for protective measures and “as many layers of protection as possible” including vaccination, masks and improving ventilation in these spaces.
“We are going into winter, we will be indoors, and we will be dining in restaurants where there is zero ventilation.
“I’ve been there, I’ve measured this, I’ve seen how high concentrations of carbon dioxide are in many naturally ventilated venues, which means relying on opening windows.
“But it is too cold during winter so the windows are closed and the restaurants are full of 30,40,50 people who are next to each other at a table and we are spending say, two hours dining.”
The issue for many surrounding ventilation is cost and political red tape but scientists continue to push for change.
“Ventilation or filtration of indoor air is really key because it takes the onus of responsibility away from the individual and puts it on the people in charge of the building,” Professor Greenhalgh said.
Professor Greenhalgh referenced Belgium’s recent “ventilation plan” which means all places open to the public, such as bars, restaurants, cinemas, theatres and gyms, will be safer for the public.
“I am very happy that the Government has found an agreement for a legal framework that will require all publicly accessible places to continue to monitor their air quality,” Minister of Health Frank Vandenbroucke told De Morgen.
“They must all have a CO2 meter.”
That same CO2 meter is exactly what Morawska carries.
“I have been to Melbourne last week, Sydney two weeks ago, so I’ve been to public places, but if I’m in public places first of all I check the concentration,” she said during an interview update from Queensland.
More Coverage
“If the concentration is really low I don’t wear a mask but if I have to be there and it’s high, I will wear a mask all the time.
“The complexity with this is that there is not one authority responsible for this, but many people and government departments because if you are dealing with schools, it’s the Department of Education, if you are dealing with business, there’s another ministry, if you are dealing with aged care, it’s the Health Department. Each ministry is responsible for something else.
“In Australia, it has been extremely patchy and nothing much has been happening.”





