Urgent warning over ‘relentless’ health issue
By 2030, almost 300,000 Australians will be faced with this debilitating health issue, an expert has warned.
OPINION
Imagine living with relentless gut pain, fatigue, and uncertainty – seeing doctor after doctor with no clear answers.
For patients with inflammatory bowel disease (IBD), every flare-up brings fear: Will it pass, or spiral out of control? Will it mean stronger medications or surgery?
The unpredictability is exhausting, leaving patients feeling powerless.
The latest State of the Nation Report highlights a stark reality: by 2030, almost 300,000 Australians will face this challenge.
Beyond the physical toll, the financial burden is staggering – lost wages and medical costs will reach $7.8 billion by 2025.
The report also reveals that patients wait an average of 1.5 years for a diagnosis and another three years to reach remission. These delays worsen outcomes and drive-up healthcare costs.
Despite advances in treatment, clinicians still lack the tools to make fully informed decisions.
Without clearer insights, treatment adjustments are delayed, care becomes less effective, and patients continue to suffer unnecessarily.

To change the trajectory of IBD care, we need earlier detection, more personalised treatment, and new treatment options.
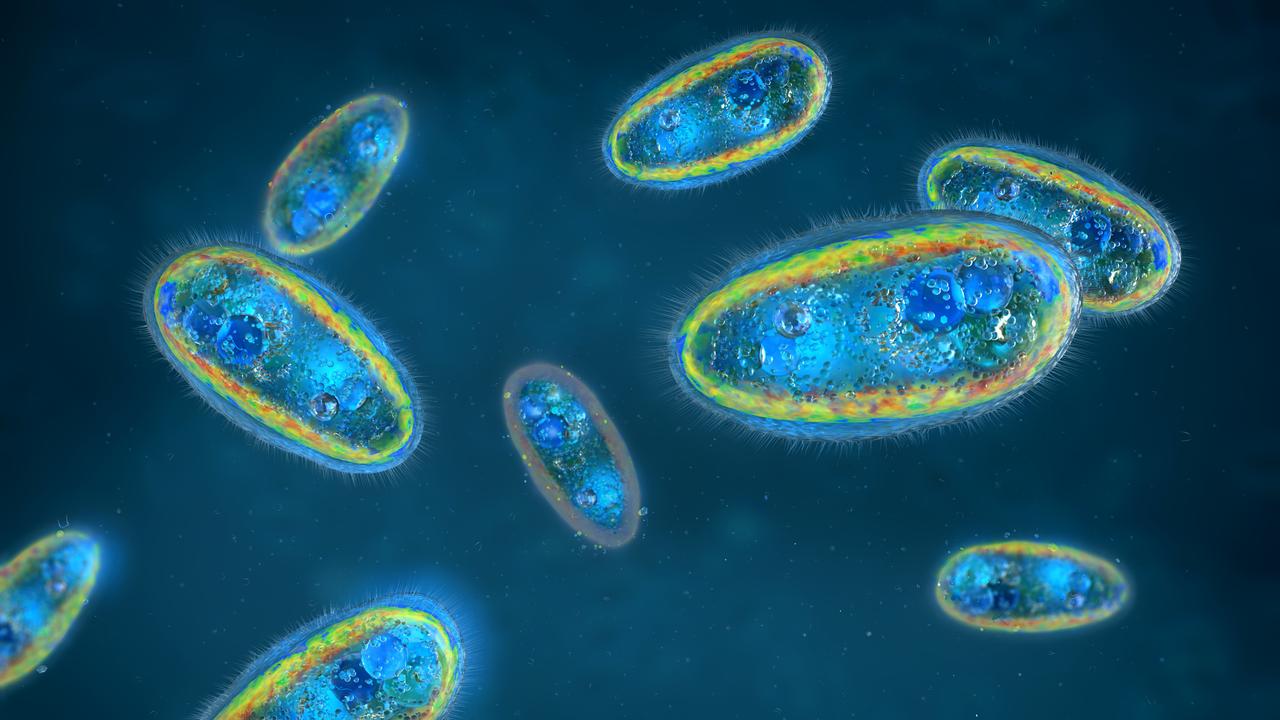
New research is uncovering a potential connection between the microbiome, infections and IBD flares, suggesting that pathogens or microbial imbalances may contribute to disease progression and symptom severity.
Ongoing clinical research suggests that IBD patients in flare-ups test positive for infections significantly more often than those in remission. These insights could lead to improved patient management and treatment outcomes. For clinicians, better diagnostics mean smarter decisions, and improved pathogen detection may help differentiate between IBD flares and pathogens driving inflammation – potentially leading to more targeted treatment and better outcomes for patients.
This is where MetaPanel changes the equation. Unlike traditional pathogen tests, which are limited to predefined targets, MetaPanel detects a broad range of organisms which can cause infection – bacteria, viruses, fungi, microsporidia and parasites – which may provide a clearer picture of what’s driving symptoms.
With this level of precision, clinicians now have a new tool to evaluate gastrointestinal infection as a factor and refine treatment plans, prevent unnecessary interventions, and deliver faster, more effective care when managing patients with chronic gastrointestinal symptoms of unknown cause.
In a study of over 650 patients, MetaPanel identified disease-causing pathogens in 21 per cent of cases. A total of 37 different pathogens were detected, many of which are not identifiable through standard pathology tests.
These findings reinforce the growing evidence that infections may play a larger role in chronic gastrointestinal conditions than previously recognised.
IBD treatment today mainly focuses on suppressing acute inflammatory responses, but not all patients respond, long-term use carries risks, and many patients fail to achieve long-term remission. That’s why we’re developing next-generation therapeutics that harness health-associated bacterial strains from the human gut that may restore immune balance and promote gut healing.

Our lead drug candidate, MAP 315, has successfully completed a Phase 1 clinical trial, where it was safe and well tolerated. A Phase 2 trial is now in development, bringing us closer to offering new treatment options that promote gut health rather than just dampening immune responses.
Transforming IBD care isn’t just about breakthroughs – it’s about ensuring they reach clinicians and patients. We collaborate with gastroenterologists, GPs, infectious disease specialists and researchers to bring innovation into practice. With smarter diagnostics and emerging treatments, IBD care is becoming more precise and patient centred.
The future of Gastrointestinal (GI) diagnostics is evolving. MetaPanel is available now and already offering broader insights than conventional tests, helping patients with complex GI conditions get the answers they need.
Associate Professor Lutz Krause is the the Chief Scientific Officer at Microba and an internationally recognised expert in the application of big data methods to understand molecular biology.