‘Life and death situation’: Unvaccinated mum challenges hospital’s ‘no jab, no heart’ policy
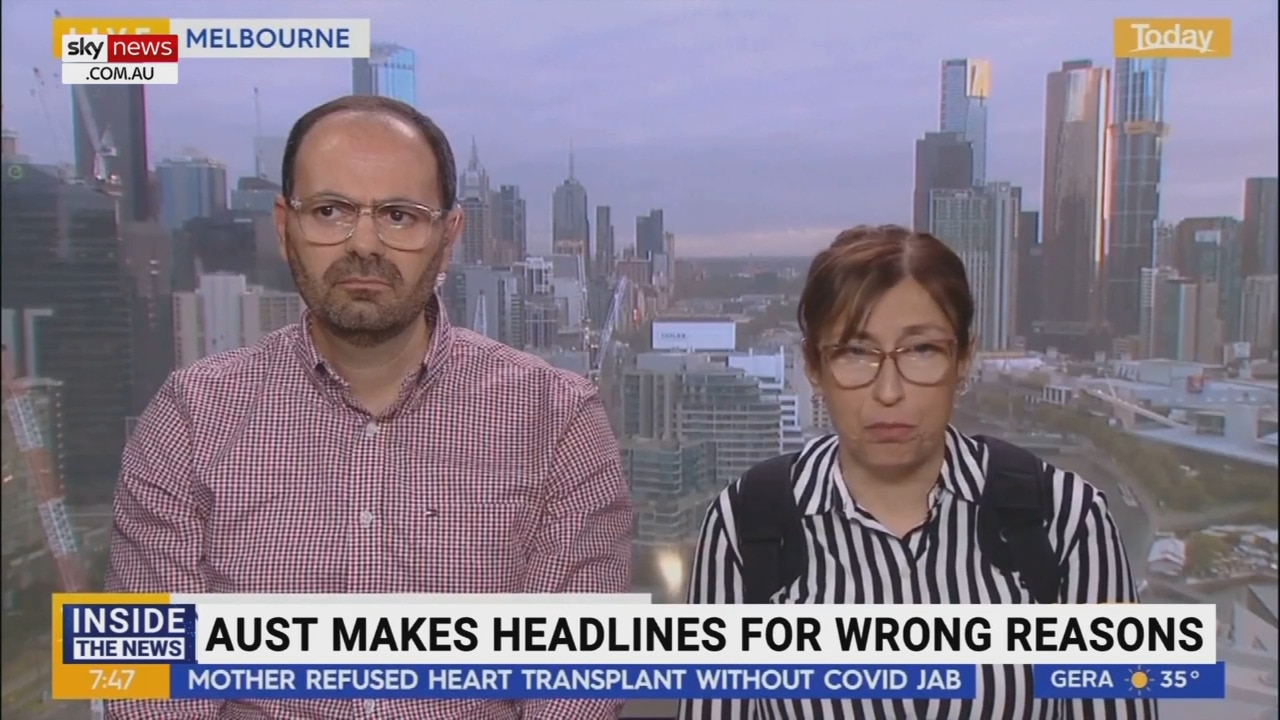
A mum-of-two being denied a lifesaving transplant under a “no jab, no heart” policy claims she is being “punished” for refusing the Covid vaccine.
EXCLUSIVE
A Melbourne mum being denied a lifesaving transplant under a “no jab, no heart” policy has accused the hospital of “ideological” discrimination for refusing the Covid vaccine.
Vicki Derderian, 47, has been on mechanical life support since 2020 after her heart failed and is desperate for a transplant, but The Alfred Hospital deemed her ineligible to be placed on the organ donor waiting list because she is not vaccinated against Covid.
“I think it’s a form of punishment,” she said.
“They’re set in their ways — basically it’s ‘no jab, no heart’. There is no long-term study on the efficacy of vaccines on pre- and post-transplant patients. I have a legal exemption from ATAGI which they are refusing to acknowledge.”
Despite widespread public attention on her case, Alfred Health is refusing to budge, offering only to meet with Ms Derderian to discuss her “vaccination concerns”.

The mother-of-two suffers from a rare auto-immune disorder called sarcoidosis and is concerned about the risk of heart conditions such as myocarditis or pericarditis associated with the Pfizer and Moderna mRNA vaccines.
Myocarditis, inflammation of the heart, is a known but rare side effect of the mRNA vaccines, reported in around two out of every 100,000 people but more commonly among boys and young men.
Ms Derderian is challenging Alfred Health’s decision in the Victorian Civil and Administrative Tribunal (VCAT), alleging discrimination under the Equal Opportunity Act 2010.
The case was heard over four days between October and March, with closing submissions on Tuesday this week.
Advocate Serene Teffaha, who is representing Ms Derderian, said during the proceedings she asked Alfred Health’s representatives if they were “aware of deaths and serious adverse events” from the vaccines but was told they “haven’t observed” anything.
But in March last year, Deakin University student Natalie Boyce, 21, died at The Alfred from heart complications, five weeks after receiving the Moderna booster shot.

Ms Boyce was the 14th death officially recognised by the Therapeutic Goods Administration (TGA) as being linked to Covid vaccines — and the only one Australia’s medicines regulator has linked to either of the mRNA shots.
Ms Teffaha said despite the fact that it occurred “on their own turf”, the “tragic death was neither revealed nor mentioned” by Alfred Health and she only later read about it in the media.
“They did not appear to acknowledge that serious adverse events and deaths were a real problem and that it happened at their own hospital,” she said.
“There is a glaring irony in asking someone who’s starting off with a serious heart condition to take a vaccine that has a risk of creating a serious heart condition. It’s logically unbelievable.”
In her closing submission, Ms Teffaha argued that the Covid vaccination requirement was discriminatory as it did not apply equally to all patients, such as those receiving chemotherapy or bone marrow transplants, “despite the fact that some of those patients will be placed on immunosuppressive therapies”.
During the proceedings, Alfred Health deputy director and head of echocardiography Dr Angeline Leet was asked the reason for distinguishing between vaccinating heart transplant patients and others who require immunosuppression.

“The reason is because after heart transplantation the body’s ability to form an immune response to the Covid-19 pathogen is reduced, and because we have seen poorer outcomes in these patients who develop Covid-19 after heart transplantation it is important that everything possible that can be done to reduce the severity of the illness post heart transplant should be done in preparation for that,” she said.
Asked whether the same would be true for patients undergoing chemotherapy, Dr Leet replied that was “outside of my area of expertise”.
Ms Teffaha argued there was an “ideological reason” behind the vaccination requirement.
“Does the expectation on the applicant to ‘treasure’ the heart and the respondent’s ‘stewardship’ of the donor heart also extend to the numerous risk factors associated with heart disease post-transplant, including demands on the applicant to control her diet, refrain from private activity such as drinking or smoking or eating fast foods or the level of exercise she undertakes?” she said in her submission.
“Confining this ‘stewardship’ to the vaccination issue alone supports the applicant’s contention that the requirement is ideologically justified as an isolated demand on the small group of patients presenting with the protected attribute.”

In a letter to Liberal Senator Gerard Rennick last month, Alfred Health acting chief executive Simone Alexander said the matter was “complex and emotive not only for Ms Derderian and her family, but also for other patients and their loved ones undergoing organ transplantation”.
“Clinical treatment options for patients waiting to receive specialised treatment, such as a heart transplants, carry significant risk for post-transplant complications,” she wrote.
“To ensure a uniform approach and the best possible outcomes for patients, the vaccination guidance for potential organ transplant recipients, is set through the Transplantation Society of Australia and New Zealand (TSANZ) and the Australian Immunisation Handbook.”
Ms Alexander said Alfred Health was “continuing to work through treatment options with Ms Derderian and her family”, which included “further opportunities to meet with our infectious diseases team to discuss treatment options and her vaccination concerns”.
The TSANZ clinical guidelines list “noncompliance with recommended pre-transplantation vaccinations” under “exclusion criteria”.

“The seroconversion rate after vaccinations is significantly higher in the non-immunosuppressed population compared to vaccination in immunosuppressed solid organ transplant recipients,” the guidelines state.
“It is therefore critical that potential transplant recipients are vaccinated before transplantation, to enable them to develop adequate immune responses to the pathogen. Rates of Covid-19 infection, severity of illness and mortality rates have been reported to be lower in the fully vaccinated transplant recipients, compared to non or partially vaccinated recipients.”
Ms Derderian, who wears the ventricular assist device at all times, said it was a “life and death situation”.
“I don’t know how long this machine will sustain me,” she said.
“I don’t really have quality of life in terms of what I can do. I’m carrying 5kg on my back, all day every day. I can’t do anything quickly, I get dizzy. A 1km walk is the most I can manage, also because of my shoulders I’m in so much pain all the time. I’m prone to infection, I need assistance showering. I need to change the batteries every 17 hours, I have to carry spare ones with me in case they break down. I need electricity at all times. It’s like I’m a bionic woman.”

She added, “A heart transplant is the only way for me to have a normal life.”
In a statement, an Alfred Health spokesman said the hospital “always provides the best possible patient care that is supported by current clinical evidence and practice”.
“While Ms Derderian remains a patient of The Alfred, she is not a current inpatient,” he said.
“We respect patients’ rights to privacy and are careful about commenting on individual patient circumstances. Transplantation is a complex medical procedure, and detailed guidelines for Australia and New Zealand ensure a uniform approach to determining a person’s suitability for organ transplantation.”
He added that while adherence to vaccination schedules was “one consideration for identifying a transplant candidate”, there were “also a range of other medical factors that ultimately determine whether a patient can be placed on a transplant waiting list”.






