How the coronavirus was able to spread so quickly at Crossroads Hotel
Usually, COVID-19 cases take days to become infections - but something strange is happening in NSW and it has experts very concerned.
The coronavirus in NSW is spreading at a “very fast” rate and some people may have passed on the virus as quickly as one day after being infected.
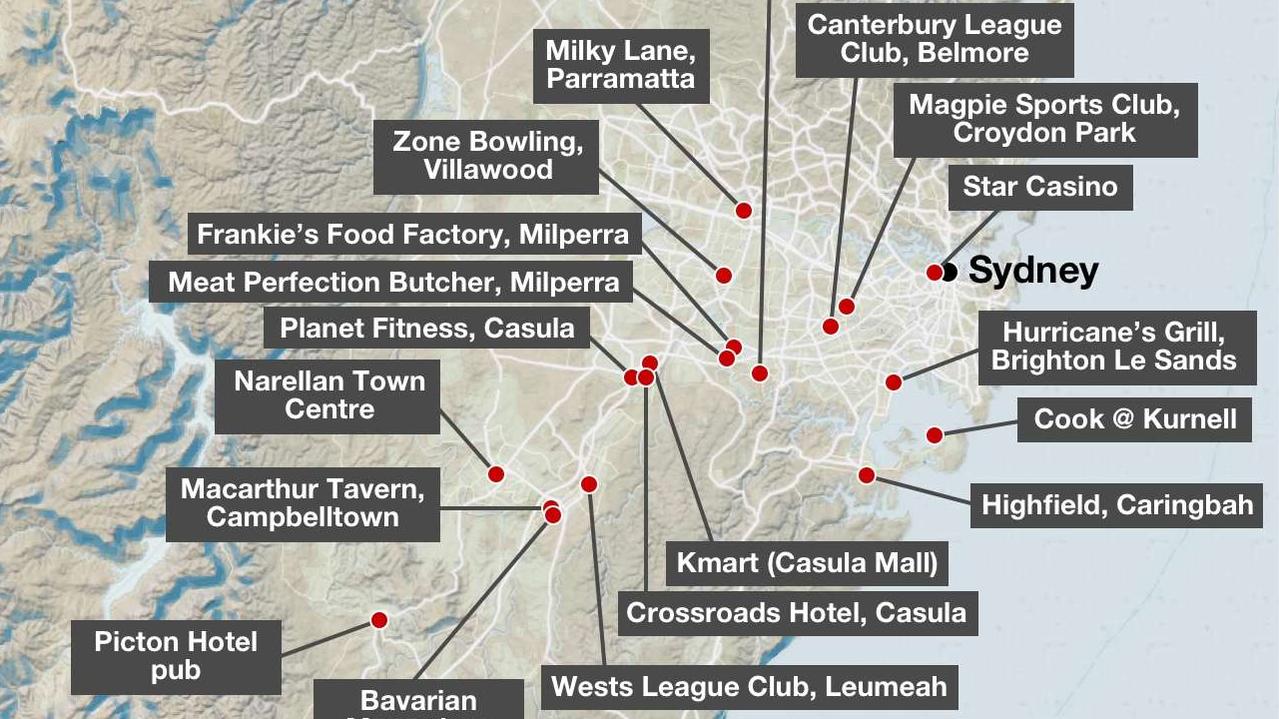
So far 19 people who visited Sydney’s Crossroads Hotel in Casula have got the coronavirus, and another 25 were infected through being close contacts of positive cases or going to the Planet Fitness gym, where another positive case worked out.
In less than two weeks, the virus has also spread to at least two “tertiary” cases — people who got the virus from the contact of a contact.
NSW Chief Health Officer Dr Kerry Chant said the tertiary cases highlighted the importance of diagnosing people really quickly.
“I think what’s been interesting is we’ve seen some acquisition which has been very short,” she told reporters on Wednesday, explaining that the incubation period for the disease was normally between one and 14 days.
“So people have developed the symptoms more towards the one day period than the 14,” she said.
“It gives you very little time for the contact traces because you’ve got to get your case diagnosed, and then you’ve got to lock down those contacts … I think it just highlights the speed.”
Professor Michael Kidd, the country’s deputy chief medical officer, today described the behaviour of COVID-19 in one patient as “unusual”.
“(The NSW patient) appears to have become infectious within 24 hours of being infected with COVID-19,” Professor Kidd said.
Typically, people infected with COVID-19 will develop symptoms within five to seven days and are usually infectious 24 hours prior to feeling ill.
Sydneysiders were first warned of the potential Crossroads cluster on Friday and in less than a week, it has now been linked to more than 40 cases.
Authorities revealed this week that a Melbourne man who travelled to Sydney on June 30 was likely ‘patient zero’. This man had gone to the pub for a party on July 3 with work colleagues, some of whom were also likely infected.
A week later authorities identified the pub as a potential hotspot of infection after two coronavirus cases both reported they had been there.
“My message to you in the community would be, if you’ve got a sore throat today, don’t wait for two days to get it diagnosed,” Dr Chant said. “Work with us, go get tested on day one because every day you can give us allows us to stop that spread.”
RELATED: Follow the latest coronavirus updates
RELATED: Mystery virus case in second NSW city

‘HE DIDN’T THINK HE WAS UNWELL’
While some people may be surprised at how easily the coronavirus was spread among pub patrons, Professor Peter Collignon of the Australian National University, said it fits with how the virus operates.
“Most outbreaks in Australia, such as in nursing homes, have begun with people with mild illness going to work,” he said.
Authorities said the Melbourne man didn’t think he was particularly unwell at the time or that he was sick with COVID-19.
But Prof Collignon said people who had mild symptoms were probably the most likely to spread the disease.
In the days before the group headed to the pub, the virus was transmitted to the man’s colleagues, who then likely helped spread it more widely at the venue, including to a staff member.
While it is possible for the virus to be spread through surfaces, Prof Collignon said it was probably less about infected beer glasses and more about close contact.
“The biggest risk is being in someone’s face,” he said.
The virus is mostly spread through droplets that spray when people talk, sneeze or cough.
This is one of the reasons pubs have been identified as higher risk venues because people often speak more loudly to be heard over the music, which sprays droplets further.
People also tend stand close together and mingle with others, which is why authorities have restricted venues to seated patrons only.
“It makes sense that staff got infected, and they were then likely a vehicle to spread it to others because they were in close proximity,” Prof Collignon said.
RELATED: Another 20 NSW venues put on high alert for COVID-19
RELATED: Superspreader scenario Australia must avoid
SUPERSPREADER’S HIGH INFECTION LEVEL
A superspreader may also have played a part.
“We’ve got a young bloke from that latest cluster … he had one of the highest infection levels we’ve ever seen,” NSW Health Minister Brad Hazzard told 2GB’s Ben Fordham on Thursday.
“His viral load was quite capable of spreading it to anybody near him … we all need to be on high alert.”
Superspreaders are people who are more likely to spread the illness due to a combination of factors including the characteristics of the disease, the patient’s biology and their environment or behaviour.
“Some infected individuals might shed more virus into the environment than others if their immune system has trouble subduing the invader,” Professor of Entomology and Director of the Centre for Infectious Disease Dynamics at Pennsylvania State University, Elizabeth McGraw, wrote in a piece for The Conversation.
“Additionally, asymptomatic individuals – up to 50 per cent of all those who get COVID-19 – will continue their normal activities, inadvertently infecting more people.”
One study estimated that 20 per cent of all those infected with the coronavirus were responsible for 80 per cent of all local transmission.
Prof Collignon said one person had also been responsible for an outbreak in Korea that saw one or two hundred people infected in bars.
“You tend to think your friends and family are safe,” he said. “But all the evidence suggests the biggest risk is being too close to people — less than 1.5 metres — when you are indoors.
“Some people have higher doses of the virus but it’s mostly about close contact, not that you shouldn’t continue to wash your hands.
“It’s that complacency that’s the problem.”




