Dr Zac Turner on the biggest monkeypox worry for Australians
A commonly held belief about the monkeypox outbreak risks leaving us with a blind spot that allows it to spread further.

Welcome to Ask Doctor Zac, a weekly column from news.com.au. This week, Dr Zac Turner talks about how the stigma associated with the monkeypox outbreak is dangerous for all Australians and how the outbreak is managed.
QUESTION:
Hi Dr Zac, I am bound for Europe to embark on a cruise, and I cannot wait! Except there is one thing that’s concerning me. In the last couple of weeks there has been so much more talk about monkeypox exploding across Europe in gay communities that it’s making me nervous.
It seems our Government doesn’t care as much as others – the US government just authorised vaccines for use but Australia hasn’t.
Is there a reason why the Australian government is not being more proactive? Have we not learned from the HIV/AIDS epidemic? Is their inaction because the gay community shouldn’t be worried about monkeypox here in Australia? I hear we already have 45 cases here in Australia – is it only a matter of time until we have similar numbers as Europe? — Benjamin, Adelaide
ANSWER:
Let’s start by saying that whilst monkeypox is a virus it isn’t like HIV/AIDS. Nor is it like Human Papilloma Virus (HPV) – a big cause of cervical cancer, which is often spread from infected asymptomatic men to women. Just like any virus it spreads in its own unique way and has its own symptoms and treatments. I believe at-risk groups should receive increased education and fast-tracked treatment (in this case, there is a vaccine available) to avoid unnecessary consequences especially to the immunosuppressed in our communities.
Thankfully monkeypox needing skin-to-skin makes it far less infectious and communicable than Covid-19. We do know that it can be spread between infected animals (monkeys originally, hence the name and prevalence in countries where these animals live) and infected individuals. However, compared to many other viruses in today’s society:
• it is difficult to transmit
• it often doesn’t need any treatment as it will resolve on its own
• and we do have current vaccines that are effective both prophylactically (before being exposed) and post-exposure.

We do know that many diseases including this virus are having an easier time spreading in part due to climate changes that enable viruses normally only found in very hot and humid conditions (like those of Central Africa) to survive now in Europe, the USA and Australia. Whilst we still don’t know the natural reservoir for monkeypox in the countries where it has been around for many years, it can be assumed that the ease of travel nowadays will make virus containment and control a bigger priority.
Monkeypox has been around for more than 70 years in various countries and in relation to the recent global outbreak, there have been zero deaths associated with it in countries outside of where it is endemic (meaning where it has been for decades) – so this is reassuring.
While it can look pretty nasty when people are infected and get some of the boils and rashes, remember, so does chickenpox if you’ve had that previously. Coxsackie Virus, also called “hand, foot and mouth disease”, affects daycare centres and children all around the world and looks terrible, is highly contagious and just like monkeypox has a swift recovery with very few long term issues.
It is unhelpful at best, and extremely harmful at worst, to paint, label or stigmatise a virus to any individuals, groups, countries, cultures or genders. The fact this virus, which has been around for such a long time, could be and is being painted as a “gay virus” is a very dangerous narrative. I’ll explain why in a moment. Misinformation on viruses has had a profound effect on people over the centuries and we must learn from these past mistakes.

Anyone can get monkeypox, but in the latest outbreak, the virus is predominantly spreading among men who have sex with men – at this stage. monkeypox isn’t considered a sexually transmitted disease though it has been recently upgraded to a “communicable disease of national significance”, which is an important move by health authorities as it will allow available resources and vaccines to be quickly disseminated.
As I’ve stated in my previous column about monkeypox, prolonged skin-to-skin contact is a leading cause of current transmission. The transmission rate for monkeypox, even with prolonged close-contact, is very low – with only about 3 per cent of contacts being infected.
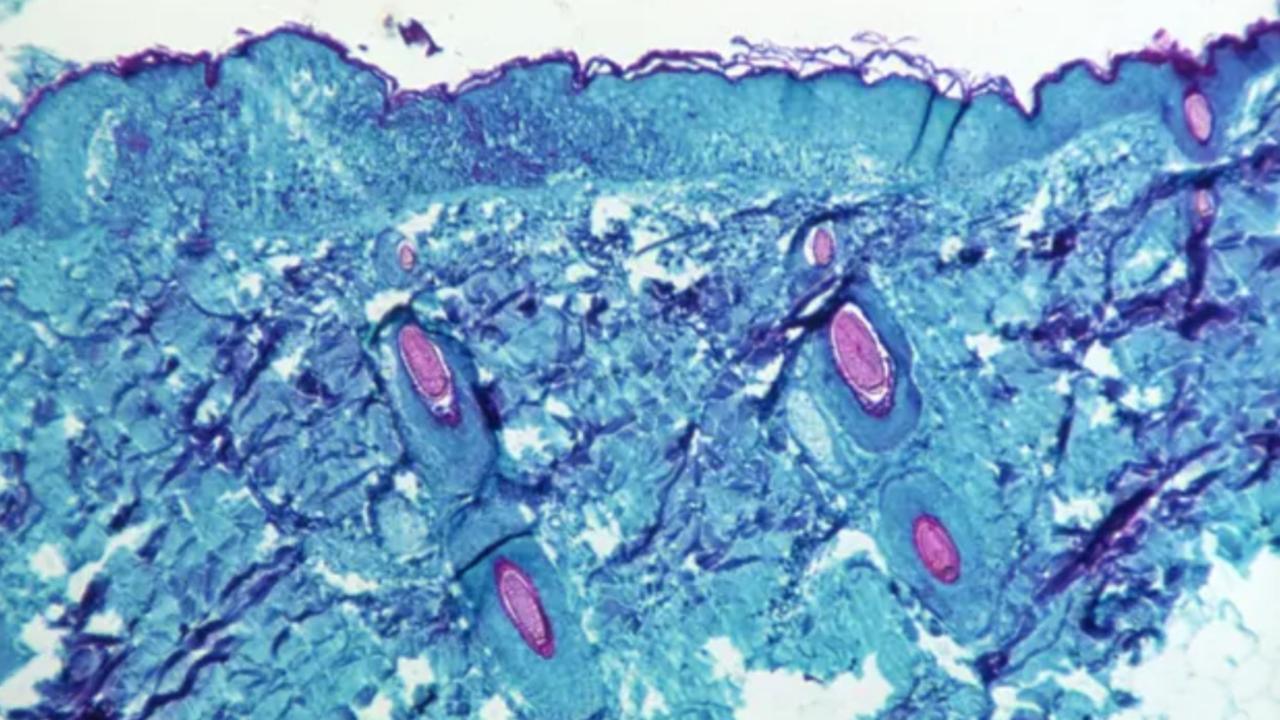
If you are one of those 3 per cent of people infected, after 5-21 days post exposure, you will generally have a fever, headache, muscle aches and your lymph nodes may also swell.
Shortly thereafter skin eruptions will often appear on your hands, feet and face. This is most likely the photos you have been seeing on the internet. As with most viruses it can result in fever and upper respiratory symptoms such as a cough or runny nose.
I do believe the Australian government should be ramping up health-communications about the virus and educating Australians on how to limit transmission. They should also be stamping out any rising stigma that this is a gay-virus, and as I’ll discuss below why fast-tracking vaccines is so important.
Although a high-proportion of cases have occurred among men who have sex with men, this could have easily been an outbreak in other networks where there is a person to person contacts – such as a football team, a nail-salon, a massage studio, a brothel, a church choir or even a child daycare. As long as there is prolonged skin-contact in the network, there is a risk for a monkeypox outbreak.
The problem with letting this stigma form is that people will believe they won’t have monkeypox because they aren’t a gay man. So if they do have the virus, they will unknowingly infect their community and its vulnerable persons. Or if their symptoms are really bad, they will refuse treatment and suffer alone because they fear their friends will label them as gay.
Now to your question about the Australian government’s hesitancy with vaccines. Let’s start out by saying there are treatments and vaccines that work – so at this stage no need to worry about waiting a year for one to be made. Just as with all medications and vaccinations that work there is a potential for side effects.
Unlike Covid-19, HPV and other viruses where the transmission is both quick and complications severe, people with monkeypox like those with Chickenpox have in the past recovered quickly and completely. Vaccinations’ benefit to risk ratio should always be discussed with a medical professional and not with your Twitter or Facebook feed. At this stage vaccinations will only be needed for individual cases and groups exposed over the incubation period and their close contacts.
I do believe the Australian government should be taking stock of its monkeypox vaccines, and be proactively supplying them accordingly to cluster areas across the country. But I don’t believe it should be publicly, and directly, targeting gay men and saying, “This virus only affects you, only you need to be vaccinated.”
Any Australian who becomes infected, needs to be vaccinated, regardless of sexuality and gender.

How to protect yourself from monkeypox
Over the last few weeks I have been keeping in touch with several colleagues overseas about their country’s access to vaccines and response to this outbreak. I am quite happy to say that I have been surprised by the level of access to foreigners who have contacted the vaccine and medical centres abroad.
At the time of writing this article I am aware of Australian citizens who have been able to arrange a vaccine whilst already overseas with a wait time as little as 3-4 days. I have some prudent advice if you are like some of my patients and friends who are going to be “doing summer in Europe” (i.e. going to festivals, clubbing or swanning about on cruises where you will be, or potentially might come into close contact with other revellers).
I would definitely recommend you book in to a GP in Australia and make sure all your vaccines are up-to-date. And if the monkeypox vaccine is not yet available to you, then check online and pre-book something abroad. And do it on your first day in a country where you can get a booking.
There are a number of measures and habits to pick up in order to limit cases in the community. I have experience working throughout Central Africa and the Congo and whilst this disease was more common in those areas, we were far more aware of the need for stringent personal hygiene. We also got vaccinated before we ventured to these areas.
Wash your hands! Just like every other virus and disease, washing your hands with soap goes a long way in limiting transmission. Alcohol hand wash works similarly well. Whilst It can probably be assumed that the cases of monkeypox patients in Australia haven’t been near monkeys or other animal vectors, we need to be especially cautious at present until we know exactly how this is being spread.
Please remember that if you are feeling unwell at all then this is the time to stay home or if you need to go out wear a mask as it will reduce the spread of droplets which can infect others. If you do end up catching monkeypox, isolate yourself from others and seek advice from medical professionals.
Benjamin, have fun on your holiday! Stay safe, get vaccinated if you can, and look out for symptoms.
Got a question:
askdrzac@conciergedoctors.com.au
Dr Zac Turner has a Bachelor of Medicine and Bachelor of Surgery from the University of Sydney. He is both a medical practitioner and a co-owner of telehealth service, Concierge Doctors. He was also a registered nurse and is also a qualified and experienced biomedical scientist along with being a PhD Candidate in Biomedical Engineering






