Australians raise almost $1 million for Covax-19 vaccine but they may be better off getting Novavax
Ordinary Aussies have contributed almost $1m to a vaccine many probably won’t even use, while others say they won’t get vaxxed with anything else.
A small group of Aussies may continue resisting vaccination indefinitely in the hopes of participating in a trial for a little-known South Australian vaccine that has so far raised almost $1 million from a GoFundMe campaign.
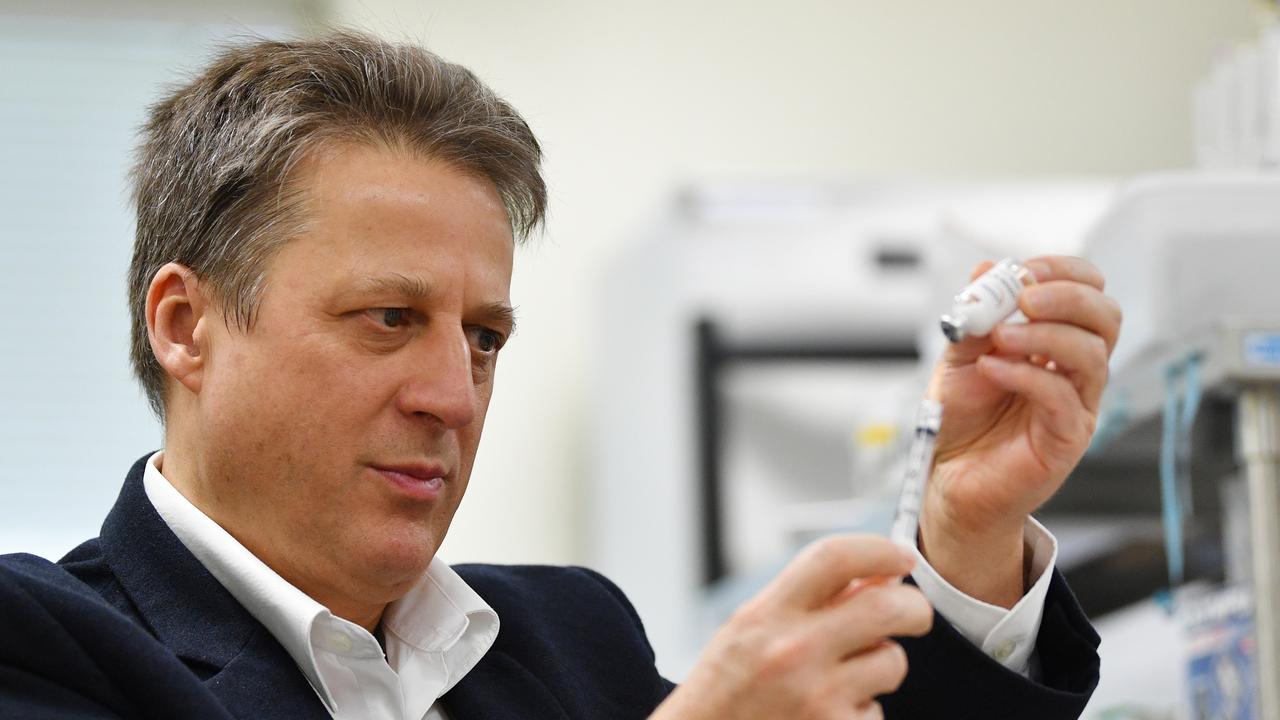
Covax-19, also known as Spikogen, is a vaccine being developed by Flinders University endocrinologist Professor Nikolai Petrovsky, who created headlines last year when he complained about having to crowdfund his project in order to give Australians access to his jab.
Some Australians are still holding out for this vaccine despite the fact that no data has been published to show it works or is safe, and even Prof Petrovsky acknowledges people may be better off getting Novavax, another protein-based vaccine due to arrive in Australia next month.
About 29,000 people have signed up to be part of a clinical trial for Covax-19 in Australia, according to Vaxine, the biotech company owned and run by Prof Petrovsky.
Some, like Ben*, a 40-something year old engineer from Adelaide, are attracted to Prof Petrovsky’s way of speaking and are sceptical of large pharmaceutical companies.
“The way he talks, to me it’s logical, rational and without bias,” Ben told news.com.au.
“The way it seems with other pharmaceutical companies, it’s belittling and censoring.”
Ben said some government information he’d read felt like “marketing brochures with cherry picked data”.
“I don’t want to risk with this new technology (mRNA), there’s been lots of negativity about it, and it seems to be being censored.”
Traditional protein-based vaccines have been seen as safer than newer mRNA technology used to make vaccines like Pfizer or Moderna, something Prof Petrovsky has also highlighted. The Vaxine website describes mRNA vaccines as “gene therapies”, something that has been debunked because the mRNA does not interact with DNA at all.
Ben said he had also begun questioning health advice after losing 26kg while eating saturated fat and intermittent fasting, things that went against recommendations at the time.
“That’s where I sit with both the government and big pharma businesses — I lack that trust,” the father-of-two said.
One person Ben is willing to trust is Prof Petrovsky, and he has signed up for the clinical trial and donated to the vaccine’s GoFundMe page, which has now raised more than $970,000.
Ben says he is willing to wait indefinitely for a dose of Covax-19 rather than be vaccinated with another vaccine, this is despite the fact that no date has been set for the trial and no data has been published to show Covax’s effectiveness in humans.
Stream the latest health news with Flash. Stay up to date with more than 20 global & local news sources. New to Flash? Try 14 days free >
While Ben hasn’t ruled out Novavax he says he would rather support an Australian product.
“In terms of Covax, the guy is from South Australia, you can’t get anymore local than that for me,” he said.
“I think as Australians we should be pushing that. Australian Howard Florey invented penicillin and I feel like this could be like another penicillin breakthrough in terms of what it could do for the world.”
However, Ben’s position also seems to be based on information about Covax’s ability to stop transmission, something that’s never been proven.
“A lot of it never made sense from day dot in terms of what I’ve heard and the data that comes out – for something that doesn’t work in terms of transmission (mRNA vaccines), that’s why I say I’m 100 per cent behind Covax because it does what a vaccine is supposed to do, it stops transmission,” Ben said.
No data about Covax-19’s effectiveness
While people like Ben believe Covax stops transmission of Covid-19, no data has been published to show this is the case.
In a Flinders press release from August last year, Prof Petrovsky was quoted as saying a study in mice and ferrets “give a hint” that Covax could “reduce the risk of transmission based on the lack of virus shedding in the noses of ferrets”.
No other evidence has been provided and even for other vaccines that have been widely used such as Pfizer, it has been difficult to prove they stop transmission, partly because new variants keep appearing that are more infectious and reduce the effectiveness of vaccines.
However, when it comes to protecting against symptomatic infections, Prof Petrovsky told news.com.au Phase 3 clinical trials in Iran showed Covax provided 60 to 65 per cent protection against the Delta variant.
This is much lower than other vaccines already on the market.
Evidence from the World Health Organisation’s Scientific Advisory Group for Emergencies (SAGE) found the Pfizer vaccine provided 90 per cent protection against symptomatic disease from Delta three months after the second dose. This only fell to 65 per cent after six months, which is why boosters are needed. It was still 90 per cent effective at preventing hospitalisations.
Novavax was found to provide 90 per cent protection against symptomatic infection in a Phase 3 study conducted in the United States and Mexico during a period when variants including Delta were in circulation.
The results of Covax-19’s trial have also never been published so it’s not possible to scrutinise them further.
‘Unhelpful’ to suggest people should wait for Covax
Infectious diseases expert Associate Professor Paul Griffin has done more than 100 clinical trials including being the principal investigator for the Novavax Phase 1 trial. He is not paid by the companies but oversees the trials on their behalf.
Prof Griffin was initially supportive of Covax-19, describing it as “most advanced of our local Covid vaccines in development” but he became concerned due to the lack of data and suggestions that people should wait for Covax to become available.
Prof Griffin, who previously also warned Australians against waiting for Novavax when mRNA vaccines became available, said suggestions people should wait for Covax-19’s trial were “unhelpful” given the efforts being made to get people vaccinated.
“People are presenting letters of intent to participate in the trial as justification for an exemption,” he told news.com.au.
“There is no clinical trial registered in this country, it’s misleading for people to think it’s an option for an approved protein-based vaccine.
“If people are waiting for a protein-based vaccine, they now have an option – Novavax – and that’s what they should get, there’s no evidence to suggest Covax-19 is better in any way.
“Given it is not approved and there is no data, we simply can’t make any claims about that vaccine that can be substantiated.”
Prof Petrovsky has acknowledged the lack of data published in scientific journals but says it is a long process and he has been focused on getting information to regulators instead.
This month Australia’s Therapeutic Goods Administration (TGA) approved Covax-19’s “provisional determination” application, which means it has been deemed eligible to apply for registration.
A spokeswoman told news.com.au the application was approved after preliminary (early) clinical data was submitted.
Prof Petrovsky said he hoped to submit the full dossier of clinical and non-clinical data to the TGA within the next month, which he described as a “massive task” that other competitors had thousands of people working on.
“I think Pfizer’s was said to be 700,000 pages, which gives you a sense of the work involved,” he said.
Prof Petrovsky said Covax had been approved as being safe for use in Iran and hoped this would be confirmed soon by the TGA.
He added that peer-reviewed results showing the vaccine was safe and effective in mice and ferrets had been published in the scientific journal Vaccine.
Data from the Phase 2 study of 400 volunteers in Iran was also submitted to a journal a few months ago but Prof Petrovsky said he did not have control over how long the review would take, and he could not to reveal the identity of the journal while the study was being assessed.
Prof Petrovsky is hopeful provisional approval from the TGA will be provided within three to six months once he submits the required data, which would allow Vaxine to market and sell its vaccine in Australia.
Novavax is a ‘good alternative’
However, Prof Petrovsky has acknowledged the approval of Novavax has changed things and it does provide a good protein-based alternative for Australians.
“If Novavax is freely available and we’re still going through the (clinical trial) process, obviously it’s our duty to make people aware if they’re not already that there’s an alternative they should explore,” he said.
“We have been supporting the field of protein-based vaccines from day one, I think they are a very good class of vaccine and they’re very effective.
“We just want people to get the vaccine that’s best for them that they’re comfortable with.”

Prof Petrovsky said a clinical trial of Covax planned for Australia not yet got ethics approval and it was unclear how long this would take.
He said he could not reveal what institution he lodged the application with but said they would look at the design of the study, which would see Covax given to unvaccinated Australians.
“Ethics committees are sometimes responsive to how they see the urgency,” he said.
With so many people now vaccinated, Prof Petrovsky said approval could take longer.
Vaxine is also now shifting its focus to the use of Covax as a booster, as well as the development of an Omicron-specific vaccine, with future trials in Australia and other countries expected.
Prof Petrovsky said these trials could be approved more quickly as they were more likely to be seen as a “cutting edge question that people want the answer to”.
“I think ultimately we are now moving to boosters and the Omicron vaccine, it’s really a matter of us filling a niche,” Prof Petrovsky said.
He said Phase 4 trials in Iran showed Covax increased neutralising antibodies by 10 to 25 times if used as a booster after people were given an AstraZeneca type vaccine or an inactivated vaccine like the ones produced in China.
“One thing we haven’t tested is (using it) as a booster for an mRNA vaccine,” he said.
Regardless of whether the trial of Covax goes ahead, Prof Petrovsky hopes that once the vaccine is approved by the TGA, people will then be able to buy it in Australia, as an alternative to Novavax if they want.
Covax won’t be rolled out as part of Australia’s nationwide vaccination program unless it also gets approval from the Australian Technical Advisory Group on Immunisation (ATAGI).

Too late for many Aussies who donated almost $1m
Prof Petrovsky acknowledges many of those who donated to the GoFundMe won’t get vaccinated with Covax, saying some supporters had already got an alternative vaccine.
“But people weren’t donating for themselves to be part of the program, it was to support the vaccine being brought back to Australia,” he said.
“That was very clear on the website.
“It’s good for Australia if the vaccine succeeds. They wanted to support this, and obviously the government haven’t done that.”
He said Vaxine had been left at a disadvantage due to a lack of government support.
While the company was provided with a $1 million Federal Government grant, Prof Petrovsky said this was very little compared to the $3 million given to the University of Queensland’s project, which was ultimately abandoned. UQ also got $10 million in funding from the State Government, as well as $3.5 million from the Paul Ramsay Foundation.
Overseas companies like Moderna and Novavax received more than $US1 billion in funding from the US Government as part of Operation Warp Speed.
Prof Petrovsky said Vaxine had been able to raise about $5 million in total, including almost $1 million from the GoFundMe, as well as grants from the US’s National Institute of Health, a UK Government partner and the George Mason University in the US.

Prof Petrovsky said a partnership with a private company in Iran helped to fund the Phase 2 and 3 clinical trials but this was delivered as “in-kind” services, not as a cash payment.
“We’ve cobbled the money together from multiple sources,” he said.
He said it generally cost between $500 million to $1 billion to get a vaccine to this stage.
“We’ve had to do the work ourselves, it’s been harder and longer but ultimately we’ve shown the value of our technology,” he said.
A Federal Department of Health spokesman told news.com.au the government had invested more than $130 million from the Medical Research Future Fund (MRFF) into funding vaccines and treatments for Covid-19.
He said Prof Petrovsky’s project was one of five projects selected to share $4.1 million in funding from the MRFF’s Biomedical Translation Bridge (BTB) program in September 2020.
Other grants are assessed by an independent expert peer review panel brought together by the National Health and Medical Research Council (NHMRC), which conducts a “world leading independent peer reviewed and ranked process”.
“The government has funded all projects deemed by the expert peer review panel to be fundable,” the spokesman said.
“This included the vaccine candidates from the University of Queensland, University of Sydney and the University of Melbourne.
“The Science and Industry Technical Advisory Group have also considered the vaccine developed by Professor Petrovsky and have not recommended further investment by the government at this stage.”
Asked whether he was worried about the money he’d donated to the GoFundMe, Ben said he thought Prof Petrovsky had not received enough support.
“I’ve got a lot more trust about where the money is going with an individual that’s rational and very genuine when he talks, rather than big pharma that have got a track record I don’t agree with,” Ben said.
“I feel in Dr Nik’s case, he has at least tried to do the right thing.
“Even if it doesn’t turn out to be what it’s promising at the moment, why wouldn’t you try when we’re still under the pump with Covid, even with a 95 per cent vaccination rate?”
‘Ultimately it’s a commercial project’
Prof Petrovsky said if the vaccine was approved it would be the first one successfully developed in Australia for 40 years.
“I think it’s morally right to be given the opportunity to prove ourselves. Obviously the approval in Iran is encouraging but people want to see it made available in Australia.”
Once the TGA approves Covax, Australians will be able to buy the vaccine, which will likely be manufactured in Iran initially.
Vaxine was hoping to manufacture the vaccine in Australia through generic medicines supplier Arrotex Pharmaceuticals, which put forward a proposal for a manufacturing hub, but this was ultimately not supported by the Federal Government.
Prof Petrovsky confirmed that as a shareholder of Vaxine, he would benefit from the sale of the vaccine.
“It’s a commercial project ultimately but Vaxine hasn’t made money for the 20 years it’s been investing in vaccines,” he said.
“If successful, I guess those profits would be used to build the company, we have always reinvested in ongoing vaccine development.”
* Not his real name






