Coronavirus v the flu: What’s the difference?
With the flu season imminent, distinguishing between coronavirus and influenza is causing plenty of confusion. This is how they differ.
Australians have been on a Google frenzy since the COVID-19 outbreak emerged as a global pandemic.
With the start of the flu season imminent, being able to distinguish coronavirus from the influenza is top of their minds.
But it has caused a state of confusion, as national chemist chains like Chemist Warehouse start to take appointments for influenza vaccines across the country.
Many are wondering if the flu vaccine will protect you against the virus at all.
One of the top questions being asked by Australians according to Google Australia’s trends is: “Is coronavirus worse than the flu?”
Coincidentally, the flu season peaks in May – the same month the COVID-19 is set to peak.
Prime Minister Scott Morrison urged calm as he described the new coronavirus as more like a “very bad flu” than SARS or MERS.
But rather than turn to your friend Google, Australians are advised to turn to official sources.
Australian National University infectious diseases physician Sanjaya Senanayake said Mr Morrison was right in his description in that both are viruses.
But they are different.
“They are both viruses but in terms of their behaviour they are slightly different.
We think that influenza is likely to be more infectious than COVID-19,” Associate Professor Senanayake said.

WHAT IS INFLUENZA?
According to the Australian government’s Heath Department, three different types of influenza viruses infect humans – types A, B and C.
Only influenza A and B cause major outbreaks and severe disease.
They are included in seasonal influenza vaccines.
Influenza C causes a common cold-like illness in children.
Only influenza A is known to have been responsible for influenza pandemics.
Influenza A and B viruses have two main proteins on the outside of the virus: the haemagglutinin (H); and the neuraminidase (N) proteins.
These proteins are referred to as ‘antigens’ because they are the structures to which our immune system responds.
New strains of influenza A and B continually emerge because of the tendency of these H and N antigens to change.
Of the influenza A viruses, only subtypes H1, H2 and H3 have been transmitted easily between humans.
Only the H1 and H3 subtypes are currently circulating causing seasonal influenza in humans.
While influenza B is essentially a human disease, influenza A viruses are found in many species.
Influenza A occurs as distinct forms or subtypes based principally on their haemagglutinin antigen, of which there are 16 different versions.
Water birds are the natural host of influenza A viruses. From time to time influenza A viruses have, however, successfully jumped the species barrier and have become established in other animals, including humans.

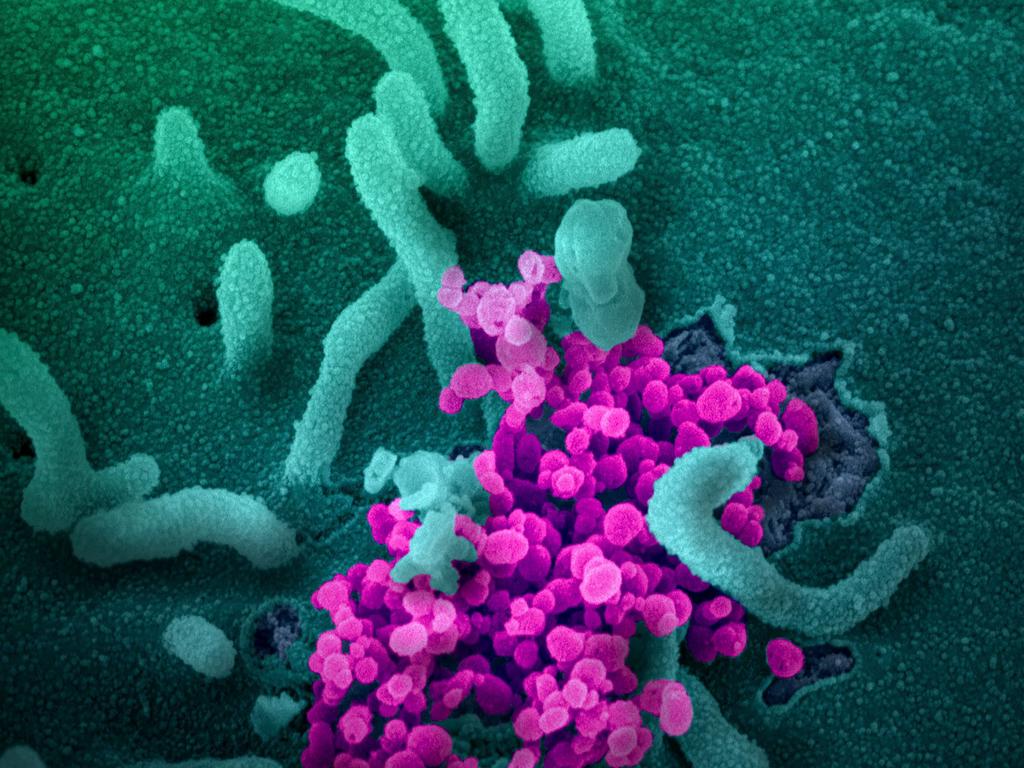
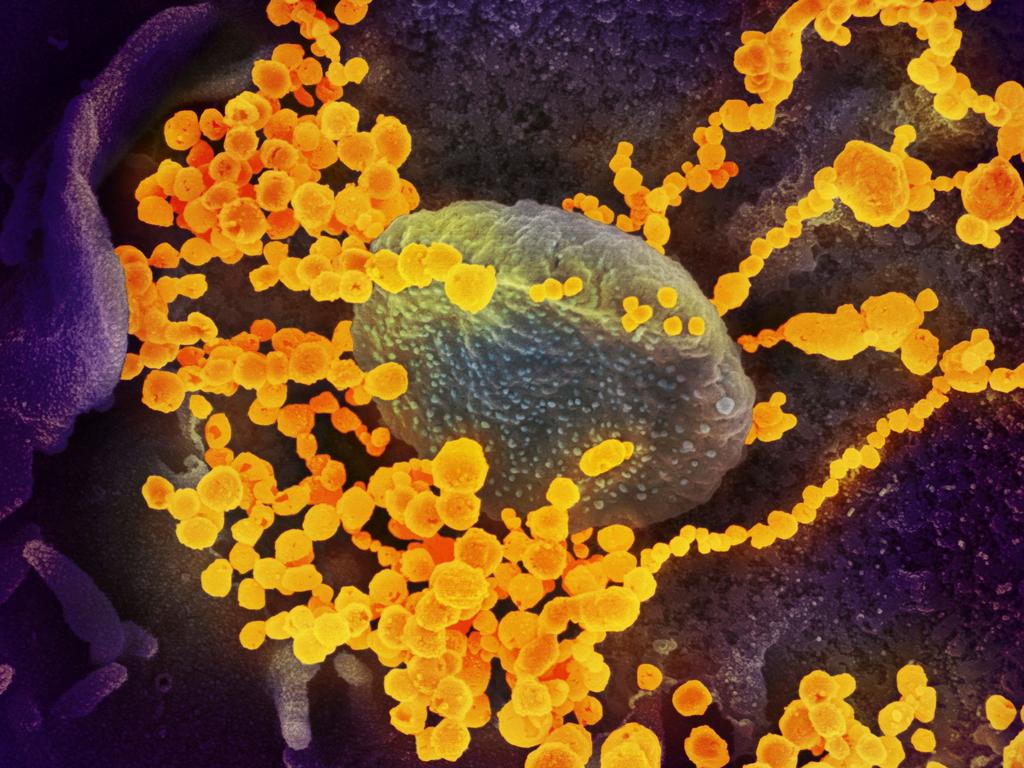
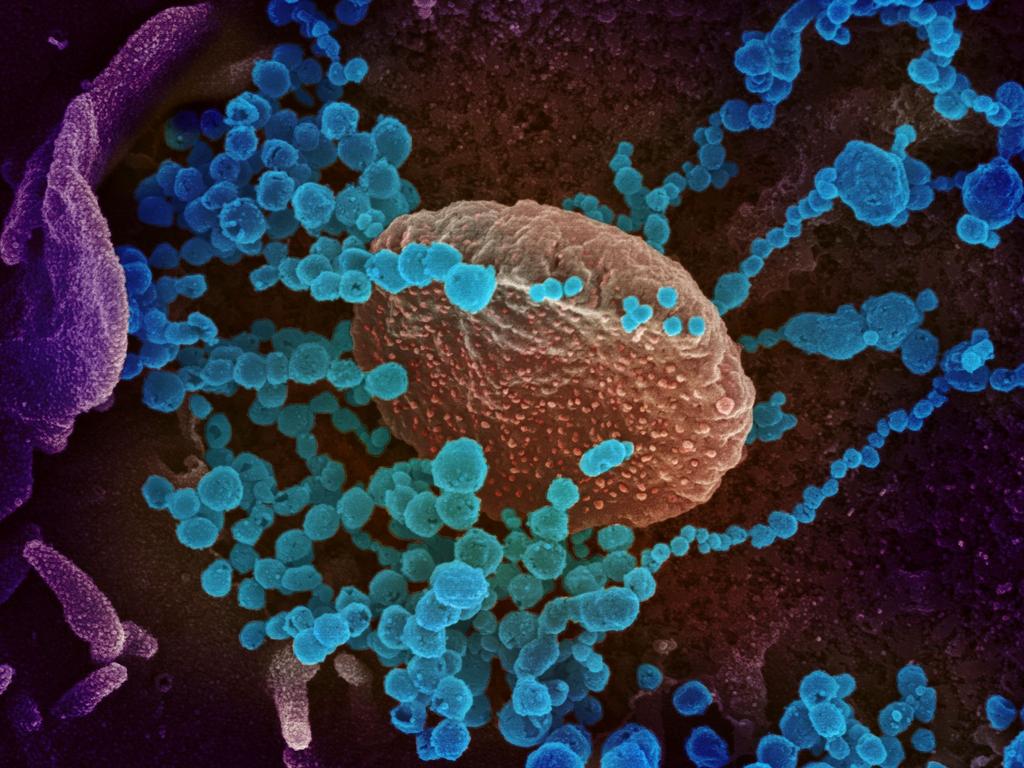
WHAT IS CORONAVIRUS?
Coronavirus is a respiratory illness caused by a new virus.
Coronaviruses are a large family of viruses that can make humans and animals sick.
It was first reported in December 2019 in Wuhan City in China.
They cause illnesses that can range from the common cold to more severe diseases.
Symptoms range from a mild cough to pneumonia. Some people recover easily, others may get very sick very quickly. There is evidence that it spreads from person to person.
You may transmit COVID-19 before you show symptoms of the virus several new studies have suggested calling into question containment policies.
And it appears to be most infectious in its early stages.
Two studies from Germany and Japan published in recent days have raised questions about Health Department advice that require only those showing symptoms to self-isolate.
The findings add weight to the gathering calls for mass public events to be cancelled to try and contain the virus.
They come as one expert calls for the flu vaccine to be made available free for everybody this year.
Researchers in Germany who studied nine patients, who were admitted to the same Munich hospital found one reason COVD 19 spreads so fast was there was very high viral shedding from the throat in the early stages of the illness.
“Together, these findings suggest a more efficient transmission of SARS-CoV-2 (COVID 19) than SARS-CoV(the 2003 SARS virus) through active pharyngeal viral shedding at a time when symptoms are still mild and typical of upper respiratory tract infection,” the research which has not been peer reviewed found.
In the 2003 SARS, it took 7 to 10 days after onset until peak concentrations the viruses RNA were reached but in COVID 19 peak concentrations were reached before day 5, and were more than 1000 times higher, the study published in medRxiv found.
Another study in Japan at Hokkaido University found the time from the onset of symptoms of COVID 19 to symptom onset in patients infected by that person was just 4 days.
Other studies have shown it takes 5-6 days for symptoms of the virus to appear and “This suggests that a substantial proportion of secondary transmission may occur prior to illness onset,” the authors wrote.
On March 2 Chief Medical Officer Professor Brendan Murphy was pressed about this issue.
He said “we do believe that there are some people whose symptoms are so mild that they may be almost unaware that they’re infected, particularly just as they become infectious. But, all of the evidence suggests that people are most infectious when they’re symptomatic.”
“So, that’s still the most important piece of advice, to isolate when you’re symptomatic.”
In Australia, it has been reported that the people most at risk of getting the virus are those who have recently been in mainland China and Iran and been in close contact with someone who is a confirmed case of coronavirus
The virus is most likely spread through:
*close contact with an infectious person
*contact with droplets from an infected person’s cough or sneeze
*touching objects or surfaces (like doorknobs or tables) that have cough or sneeze droplets from an infected person, and then touching your mouth or face
WHY THE CONFUSION?
Both can cause a worse outcome in older people with chronic health problems.
But COVID-19 appears to have a higher death rate than influenza, the expert said.
“The death rate is about 0.1 per cent for influenza,” Associate Professor Senanayake said.
“COVID-19 has varying death rates. The Chinese are saying it’s around 3 per cent but we suspect it may be lower because there are many undiagnosed cases in the community.
“Even then we think it will be lower than the 0.1 per cent of influenza.”
The symptoms can present in the same way when someone is sick: a fever, cough, sore throat and muscle aches and pain – which makes it very difficult to distinguish.
“During the flu season in winter it can be very hard to tell them apart so you have got to get a test,” he said.
“We can do a swab test from the throat, nose and look for the viruses in those ways.”
Another trending question on Google being asked by Australians is: “Can you get coronavirus twice?”
Associate Professor Senanayake said if you get COVID-19 once there is no guarantee you won’t get it again.
“We don’t know, but most likely in the short-term you won’t get it again. Whether that means in the next year or two or whether we have long-term immunity we don’t know.”
There is also uncertainty on whether the flu season will make treating Covid0129 worse.
“We don’t know but the possibility is there that if you have two infections at the one time you can get sicker,” he said.
“We certainly see people that have got two infections at the one time, so I don’t see why it couldn’t happen with COVID-19.”
About a quarter of common colds are attributed to four other types of coronaviruses. But without testing nobody knows which.
Fortunately SARS isn’t around anymore and MERS is restricted to the Middle East.
He ruled out the possibility there was a carrier in Australia prior to the outbreak in China.
“None of us are immune to it and if there was someone in Australia that had it first, they would have infected enough people large enough that someone would show up to the doctor or hospital an that would raise the alarm. So I do think it started in China,” he said.

WHAT YOU CAN DO
Associate Professor Senanayake also urged people to stop panic-buying toilet paper.
Only about three per cent of people infected with coronavirus get the runs – “That’s no reason for bulk buying toilet paper. It is a very strange phenomenon.”
“I don’t think people should panic buy at this stage or any stage in fact. There may be a situation where the government says ‘look we may need to isolate ourselves for a period, go and get some necessities’, but no panic-buying, very odd.”
The government’s advice is that everyone should practise good hygiene to protect against infections. Good hygiene includes:
*washing your hands often with soap and water
*using a tissue and cover your mouth when you cough or sneeze
*avoiding close contact with others, such as touching
If you become unwell and think you may have symptoms of coronavirus, seek medical attention.
Call ahead of time to book an appointment. Tell your doctor about your symptoms, travel history and any recent close contact with someone who has coronavirus.
If you must leave home to see your doctor, wear a surgical mask (if you have one) to protect others.
If you have serious symptoms such as difficulty breathing, call triple-0 for urgent medical help.
Originally published as Coronavirus v the flu: What’s the difference?



