Coronavirus explained: What you need to know about getting sick, treatment and future vaccines
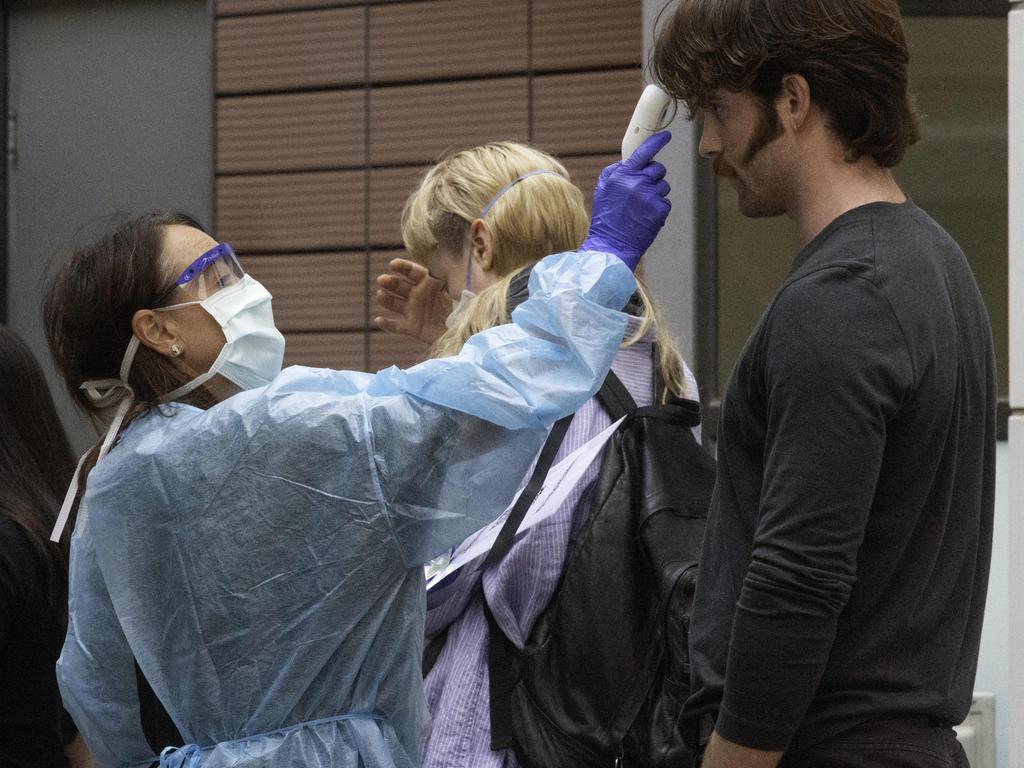
As Australia’s coronavirus cases continue to climb and new clinics are established, here’s how you can get tested.
A pop-up COVID-19 testing clinic will now be established in Bondi to help reduce the spread of the coronavirus after clusters developed within Sydney’s backpacker community.
NSW Health is now directing doctors in Sydney’s Waverley Council area, which includes suburbs such as Bondi, to send more patients for COVID-19 testing.
In most cases, if you think you need a test, don’t physically attend a health service because you may spread the virus further.
Instead, call your general practice, your local hospital or the coronavirus hotline 1800 020 080 to seek advice.
If you must leave home to see your doctor, wear a surgical mask to protect others.
The Department of Health says you will only be tested if your doctor decides you meet certain criteria, including:
- You have returned from overseas in the past 14 days and you develop respiratory illness with or without fever
- You have been in close contact with a confirmed COVID-19 case in the past 14 days and you develop respiratory illness with or without fever
- You have severe community-acquired pneumonia and there is no clear cause
- You are a healthcare worker who works directly with patients and you have a respiratory illness and a fever
The Victorian Government has set up four testing clinics attached to hospitals, some public hospitals and nine private pathology companies are providing tests in NSW, there are four public and one private testing clinic in South Australia and Queensland has also moved to establish testing clinics.
The Federal Government has set aside money for 100 coronavirus testing clinics in the community but they have not been set up yet.
The test involves a doctor or nurse taking a swab of saliva from your throat and nose to test for the virus.
CAN YOU GET COVID-19 TWICE?
The latest research into COVID-19 reinfection has shown monkeys are unable to be infected with the virus twice, giving hope that humans may build immunity.
Despite the promising results, there remains conflicting evidence among experts as to whether people can be infected multiple times.
When asked if reinfection in humans was possible, University of New South Wales microbiology professor, Peter White said: “I would think it’s unlikely in my opinion”.
Prof White pointed to the small study, by a team of Chinese researchers, which showed rhesus monkeys were protected after their first infection with SARS-CoV-2 – the virus which causes the disease COVID-19 – but said more research was needed.
The study has not yet been peer reviewed.
Prof White said if a person was to be reinfected, the symptoms would be milder than the first infection.
There have been some reports of people being apparently reinfected, but Prof White said this was possibly due to testing issues.
“There’s another possibility here, and that is that these people are not reinfected. They’ve had the same virus all along, but they had a false negative result somewhere in the middle,” he said.
“So that could confuse people to make them think that someone is cleared and then got reinfected.

“But my opinion is that reinfection would be unlikely for most people.”
Prof White added people who are immunocompromised may be at greater risk of being reinfected, but “otherwise, I think it would be unlikely”.
University of Queensland virologist Ian Mackay said it was possible people could be infected by SARS-CoV-2 “a second time, or maybe a third, a fourth and a fifth time”.
“That’s not unusual for any respiratory virus,” Professor Mackay said.
“We tend to be reinfected by these things all throughout our life, even though most of the respiratory viruses are childhood diseases that we get and show antibodies to early in life, mostly before five years of age.”
Prof Mackay agreed if someone were to be infected a subsequent time, their symptoms would be milder.
“Will we get more severe disease or severe disease again? And the answer to that should be no,” he said.
“Everything seems to be pointing us to mounting a good immune response to that first infection.
“We won’t have disease that’s anywhere near as likely to be possibly even noticed, let alone severe.”
Professor Mary-Louise McLaws, an adviser to the World Health Organisation and infection control expert, said the answer wasn’t clear cut.
“From an epidemiological point of view, the data is not clear yet,” Prof McLaws said.
Prof McLaws pointed to the cases of two elderly people who tested positive to the disease, tested negative during a subsequent test before testing positive again, but said the result could have a number of causes.
“It could be that the test failed to pick up the antibodies or the marker for the disease and that the last time they tested positive was maybe not a new infection, but actually the same infection,” she said.
“Or it could be their elderly immune system not producing the markers. It could be the test itself. It could be a relapse or it could be a second infection.”
Prof McLaws said it also wasn’t known whether a second infection with the virus would elicit a more severe or less severe reaction.
“It’s such a new disease. It’s three months old and there are many things we don’t know,” she said.
UNEXPECTED SIGN YOU MAY HAVE COVID-19
Losing your sense of smell could be one of the first signs you have COVID-19, Flinders University experts say.
Ear nose and throat (ENT) surgeons said loss of smell was reported in one in three COVID-19 patients in Korea and in Germany it was one in two patients.
Flinders University Professor Simon Carney said the virus causes swelling in the nasal passages and mucus related to smelling and could be used as an indicator of the virus in symptom-free carriers of COVID-19.
“It is these ‘silent carriers’ who may remain undetected by current screening procedures, which may explain why the disease has progressed so rapidly in so many countries around the world,” he said.
“An ENT professor in London has reported seeing a dramatic increase in patients with anosmia as their only symptom of COVID-19 infection,” he said.
As Australia struggles to contain the spread of COVID-19-10, identification of these carriers could help to slow the spread of infection.
“In the UK, ENT surgeons are pushing to have anosmia (loss of smell) highlighted as an important symptom that may signify a patient may be an asymptomatic carrier,” says Professor Carney, immediate past president of the Australia and New Zealand Rhinologic Society.
“Australia is in a position to take advantage of these findings overseas to try and ‘flatten the curve’ while we still can.”
Doctors and COVID-19 detection centres could use this subtle sign and unexplained sudden anosmia in the testing criteria, he said.
Patients should also consider calling their GP with this early symptom as a precursor for possible treatment, he said.
A major international effort is under way to control the spread of the virus and scientists and pharmaceutical companies are co-operating on an unprecedented scale to develop a vaccine and find treatments for the virus.
Coronavirus is new to humans so we have no immunity to it and it is highly infectious with older people and those with other chronic health conditions most at risk of dying from the illness.
Symptoms include fever, flu-like symptoms such as coughing, sore throat and fatigue, runny nose and shortness of breath.
Eight in 10 people who catch the virus will experience a mild case but 15 per cent will become severely ill, five per cent will become critically ill and between 1 per cent and 3.4 per cent of people will die from it.
CAN THE VIRUS PRESENT WITHOUT SYMPTOMS?
COVID-19 can present without symptoms in certain cases, particularly for children. In other cases, symptoms may be so negligible that people do not even realise they have it.
TV presenter Richard Wilkins is one of the most high-profile cases to report asymptomatic coronavirus.
Professor Peter White, virologist at the University of NSW says less than a tenth of cases of coronavirus will present without symptoms.
“There will be a cohort of people like Richard who will feel like they have no symptoms and feel fine but they might have tiny symptoms like a slight cough and will be excreting the virus in respiratory droplets but perhaps at lower levels,” he said.
The good news is, this portion of the population are less likely to spread the disease.
“The more symptomatic you are the higher the risk of spreading the virus,” Professor White said.

ARE FACE MASKS EFFECTIVE?
Face masks can be effective in protecting you against the spread of COVID-19 in certain cases.
While the official advice from the government is that face masks are not necessary, Professor Peter White, virologist at the University of NSW, said they can be useful, but hand hygiene is most effective.
“It wouldn’t do any harm [to wear a P2 mask], but you are better off using hand sanitiser and regularly washing your hands.”
Wearing a properly fitted P2 face mask in crowded areas can help protect you from inhaling infected particles from people carrying the virus.
They may also help prevent contamination by stopping people from touching their mouth and nose, Professor White said.
Surgical masks, however, are not effective in preventing the spread of the virus, he said.
WHO IS MOST AT RISK?
The elderly and people with chronic health conditions are most at risk of dying from coronavirus, while men are more susceptible than women.
Death rates are highest for those aged over 80 years of age — 21.9 per cent of them died from COVID-19 in China according to a study of over 55,000 cases.
People who had no chronic health conditions had a death rate of 1.4 per cent but those with heart disease had a death rate of 13.2 per cent, experts from the World Health Organisation (WHO) found.

Patients with COVID-19 who had diabetes had a death rate of 9.2 per cent, those with high blood pressure were 8.4 per cent, chronic respiratory disease sufferers were 8 per cent and cancer patients 7.6 per cent.
And being male also carried a higher risk of death, with the death rate among men with COVID-19 at 4.7 per cent compared to females at 2.8 per cent.
Eighty per cent of people with COVID-19 will have a mild disease, 15 per cent will have a serious illness and five per cent will become seriously ill.
Some patients will develop pneumonia and others will experience an immune system overdrive that destroys major organs.
HOW DO I AVOID INFECTION?
Coronavirus is spread via droplets from an infected person and the best way to protect yourself is to refrain from touching other people, surfaces such as doorknobs and railings, lift buttons and regularly wash your hands with soap or alcohol-based hand sanitiser.
Try not to touch your face with your hands because it can transfer the virus to your nose, mouth and eyes.
You are six times more likely to catch coronavirus from someone in your own household than from elsewhere.
University NSW and Kirby Institute biosecurity expert Professor Raina MacIntyre said new research showed the virus can survive for up to three hours in the air, two to three days on plastic and stainless steel, 24 hours on cardboard and four hours on copper.
No research has yet been done on whether it spreads via airconditioning systems.
While gloves can protect your hands from virus droplets, the droplets remain on the surface of the gloves so do not touch your face while wearing them.
Traditional infectious disease protocols call for people to keep a one metre distance to avoid infection but Professor MacIntyre said “new studies have shown droplets can travel up to six metres”.
If you have the illness you are advised to sneeze into your elbow to prevent droplets spreading, cover your mouth with a tissue when coughing and isolate yourself from others and wear a mask when around other people.
Have your flu shot so you don’t get both viruses at once as happened to many in China.
IS THERE A VACCINE?
There is a major global race to develop a vaccine US company Moderna Therapeutics already has a vaccine candidate and is recruiting people for the first human clinical trials.
The Queen Mary BioEnterprises Innovation Centre in London this week advertised for 24 volunteers to inject with the dreaded coronavirus to test possible vaccines against COVID-19.
The University of Queensland last month announced it had already discovered a vaccine candidate.
However, it could be 12-18 months before any vaccine completes safety and efficacy trials which will also show if it actually works to prevent coronavirus infection.
Then there will have to be large scale production of the vaccine with health workers on the frontline likely to be the first to receive it.

German company CureVac is working on a mobile manufacturing technology which could produce vaccine at the site of an outbreak.
American biotech Company Inovio Pharmaceuticals has announced they could start human trials on a vaccine in April and Johnson & Johnson is developing a vaccine.
US company Regeneron Pharmaceuticals, which has developed an effective treatment for ebola, hopes to have a coronavirus vaccine ready for human testing by August.
French pharmaceutical company Sanofi is developing a vaccine mixing the COVID-19 with genetic material from another harmless virus to create hybrid that can trigger an immune response without making patients sick.
Sanofi has announced it expects to have a vaccine to lab test within six months but approval would be at least three years away the company said.
WHAT IS THE TREATMENT?
There is currently no treatment for coronavirus and the main medicine used on patients in Australia has been paracetamol to reduce fever.
You may be able to treat some symptoms of the coronavirus such as fever, aches and pains and a runny nose with over the counter remedies such as paracetamol, ibuprofen, nasal spray or cough and cold remedies which combine these treatments.
Alcohol-based hand sanitiser could help in preventing the spread of the virus in your household but it is in short supply. Soap works just as well.
Tissues are useful so you can cough into them or blow your nose and dispose of the tissue to contain infection.
If you get coronavirus you will need to self-isolate at home for 14 days so if you have a chronic health condition or are taking medicines for other conditions it’s a good idea to have two weeks’ supply handy.
However, doctors and the Federal Government are urging people not to stockpile large supplies of medicines because it means other people who need them may not be able to access them.
The government hopes to introduce a new electronic prescribing system within eight weeks which means your doctor could treat you in your own home via telehealth, send the script to an online registry where it can be downloaded by your chemist, dispensed and home delivered.
We should know the outcomes of the first clinical trials of a promising antiviral treatment for COVID-19 by late next month and Australia’s medical regulator has vowed to fast track the approval of the experimental treatment if it works
A broad spectrum antiviral treatment Remdesivir developed to treat ebola is being employed against coronavirus in two clinical studies involving 760 people in China.
In January, the experimental drug was used on a 35-year-old man who was the first reported US case of COVID-19 and he showed significant improvement.
In February, Remdesivir was found to work against COVID-19 in test tubes.
World Health Organisation or WHO Assistant Director-General Bruce Aylward has said “there is only one drug right now that we think may have real efficacy and that’s Remdesivir”.
Doctors on the Gold Coast are using an existing and approved HIV treatment Kaletra (Lopinavir combined with ritonavir) to treat some severely ill coronavirus patients.
Three Chinese patients treated with the drug in January recovered and there are reports that 20 other COVID-19 patients in China tested negative for the virus after taking this treatment.
The Journal of Korean Medical Science reported last month that the virus almost disappeared in a 54-year old male with COVID-19 after he was given Kaletra.
China is also trialling chloroquine, a malaria drug that killed off the new coronavirus in test tubes.
Some COVID-19 patients have been treated with blood plasma taken from people who have recovered from COVID-19 in the hope it will give them the antibodies to the virus.
DO WE HAVE ENOUGH EQUIPMENT?
More than 1.8 million hospital beds and 650,000 intensive care beds could be needed to treat coronavirus patients in a serious outbreak, a biosecurity expert has predicted.
Australia only has 2200 ICU beds and states are working on doubling that number by repurposing other beds. Extra ventilators are also being sourced to help keep severely ill patients alive.
Professor Raina MacIntyre, head of the Biosecurity Program at UNSW’s Kirby Institute, said the bed estimate was based on a scenario where half of the population contracted the virus. It is unlikely everyone will get it simultaneously.
Leave for medical staff is being cancelled, part time health workers will be asked to increase their hours and retired workers could be asked to come back to work if the number of people with the virus expands dramatically.

The federal government has funded 100 community based fever clinics to test COVID-19 patients and reduce stress on hospitals but it could be weeks before they are up and running.
Elective surgery cases are being cancelled or shifted to private hospitals to free up room in public hospitals for potential COVID-19 patients.
The Federal Government’s own pandemic plan says in a high level outbreak of the virus access to hospital beds would have to be rationed.
Millions of masks and personal protective gear would be needed. The government already has a stockpile of 19 million masks and is expecting delivery of 54 million more, which should be sufficient.
There is a national stockpile of essential antibiotics and other drugs available.
MORE NEWS
Why school closures may not stop virus
‘30-day germ-free’ childcare as shutdown talks emerge
Should I still go on holidays in a coronavirus pandemic?
‘Second wave’ fears as virus sparks new import delays
HOW MANY PEOPLE WILL BE AFFECTED?
In the coming months and years we will all be infected by COVID-19, according to University of Queensland Professor Ian McKay.
The virus was like other coronaviruses that cause the common cold and “at some point in the coming months or years we’re all going to get infected because we’ve all been infected by these other endemic viruses,” he told News Corp papers.
It’s estimated that every person who contracts COVID-19 infects between two and 2.4 other people.
University NSW and Kirby Institute biosecurity expert Professor Raina MacIntyre said the doubling time for the virus is currently thought to be six days, meaning that if 120 people have it today 240 people will have it by next week.
NSW’s chief medical officer Dr Kerry Chant predicted 1.5 million people would contract the virus in the first wave in NSW alone.

Researchers at Western Sydney University estimated last week that by the end of the month the number of deaths from the virus worldwide would surpass 4500 and the number of confirmed cases would reach 150,000.
The world has already exceeded that figure, because of the extremely high death rate among elderly people.
And the number could be even greater, as people with the virus in places like Iran, Africa and even America have not been tested and not factored into official data.
Many people including children have such mild symptoms from the virus they may not realise they have been infected.
The longer we can keep it under control the less stress we will place on the health system and the closer we are to finding a treatment or vaccine.



