Monkeypox cases rise in Australia: What you must know
Aussies are being urged to be vigilant with cases of mpox on the rise. Here’s everything you need to know about the contagious disease.

World
Don't miss out on the headlines from World. Followed categories will be added to My News.
Cases of mpox have risen in Australia, prompting a warning from health authorities for people to be vigilant.
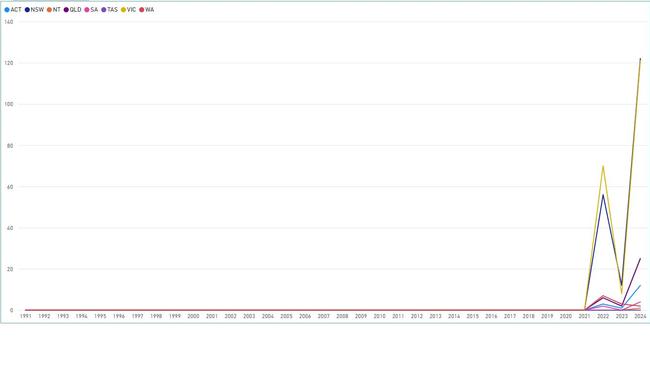
In Victoria, case numbers have hit a new peak with 121 reported this year. That is up from just eight recorded last year and 70 in 2022.
And two new cases have been reported in Western Australia.
These cases are not linked to the strain - Clade Ib - which is behind the outbreak in central and eastern Africa, which resulted in the World Health Organisation declaring a global public health emergency earlier this month.
But health experts are warning that even though it’s not the same strain, people still need to be concerned about the contagious disease, previously known as monkeypox.
They are warning eligible and at-risk people to get vaccinated and be on the lookout for symptoms.
Here’s everything you need to know.
WHAT IS MONKEYPOX?
Mpox, previously known as monkeypox, is a viral disease that historically occurred in predominantly tropical rainforests of Central and West Africa, according to the Australian Department of Health’s website.
It is a zoonotic disease, which means it can spread between animals and humans.
Mpox belongs to the same family of viruses that causes smallpox.
HOW IS MPOX TRANSMITTED?
Mpox is a viral disease that can been transmitted to humans by infected animals, and can also be passed from human to human through close physical contact.
A person with mpox is thought to be infectious from the time they develop any symptoms until all scabs have healed and a fresh layer of skin has formed. This may take several weeks.
Transmission between people can occur through close contact with rashes, blisters or sores on the skin; body fluids, including respiratory droplets from coughing or sneezing; contaminated objects such as linen and towels.
Transmission through respiratory droplets (for example coughing or sneezing) is less common and usually only happens if there is prolonged face-to-face contact.
The virus can also pass to the foetus via the placenta during pregnancy.
It was first discovered in humans in 1970 in DR Congo, causing fever, muscular aches and large boil-like skin lesions.
WHAT ARE THE SYMPTOMS OF MONKEYPOX?
The Clade Ib strain causes skin rashes across the whole body, unlike other strains where lesions and rashes are usually limited to the mouth, face and genitalia.
Symptoms begin five to 21 days after exposure to the virus.

WHO IS AT RISK?
People who have had close physical contact with an mpox case and travellers returning from, or going to, countries with confirmed cases
HOW LONG DOES MONKEY POX LAST?
Mpox causes signs and symptoms which usually begin within a week but can start 1–21 days after exposure. Symptoms typically last 2–4 weeks but may last longer in someone with a weakened immune system.
MONKEYPOX IN AUSTRALIA IS ON THE RISE
So far this year, 287 cases have been reported in Australia, which is up from 26 the previous year, according to the National Notifiable Disease Surveillance System managed by the Department of Health.
NSW has reported the highest number of cases at 122, followed closely by Victoria with 121.
There have been 25 reported cases of mpox in Queensland, 12 in the ACT, four in South Australia, two in WA and one in the NT.
Earlier this month, NSW Health urged the public to be aware of symptoms of mpox following a recent increase in infections, mostly impacting men who have sex with men.
There was previously a significant mpox outbreak in 2022, with a total of 144 cases across Australia.
All bar one case since 2022 have been in males, most commonly those aged 30-35 years old.
WHAT ARE AUSSIE EXPERTS SAYING?
Victorian chief health officer Dr Clare Looker issued a warning to Victorians on Wednesday, saying cases in the state “were on the rise”.
“A subclade known as Clade IIb, has been largely circulating since 2022 in the global mpox outbreak, mostly impacting gay, bisexual, and other men who have sex with men,” she said.
“All infections reported in Victoria to date have been caused by Clade IIb.”
She urged people to get vaccinated to protect themselves against the Clade IIb strain that is responsible for surge in cases here.
Communicable Disease Control director at WA Health, Paul Armstrong, urged high-risk groups to get tested if they suspected they might have the disease.
“Mpox infections have been increasing in Australia over the past few months – particularly among sexually active men who have sex with men and through higher risk activities such as casual sex and multiple partners,” Dr Armstrong told The West Australian.
“If you have any symptoms suggestive of mpox – even if they are mild and even if you have had the mpox vaccine – you should contact your GP or sexual health service for an appointment.
“Wear a mask, call ahead and cover up any rashes, bumps or pimple-like sores.”
WHAT IS AN INTERNATIONAL PUBLIC HEALTH EMERGENCY?
A public health emergency of international concern (PHEIC) is the highest alarm the WHO can sound and allows Tedros Adhanom Ghebreyesus to trigger emergency responses under the International Health Regulations.
A PHEIC has only been declared seven times since 2009: over H1N1 swine flu, poliovirus, ebola, zika virus, ebola again, Covid-19 and mpox.

WHY HAS MPOX BEEN DECLARED A GLOBAL EMERGENCY?
Since September 2023, a different strain of mpox, the Clade Ib subclade, has been surging in the Democratic Republic of Congo.
On July 11, Tedros Adhanom Ghebreyesus said more than 11,000 cases and 445 deaths had been reported in the giant African state this year, with children the most affected.
The disease has since spread to neighbouring countries.
The African Union health agency, Africa CDC, registered 14,479 confirmed and suspected cases of the strain and 455 deaths in DRC as of August 3, representing a mortality rate of around three per cent.
But researchers in the vast Central African nation say the mortality rate from the strain can be as much as 10 per cent among children.
In mid-August, Sweden recorded its first case of the more contagious variant of mpox, marking the first time it has been found outside Africa.
Director-general of the Swedish Public Health Agency Olivia Wigzell revealed that the person contracted the infection while in a region of Africa experiencing a significant outbreak of the disease.
WHEN WAS THE LAST TIME MPOX WAS DECLARED A GLOBAL EMERGENCY?
In May 2022, mpox infections surged worldwide, mostly affecting gay and bisexual men, due to the Clade IIb subclade.
The outbreak led the WHO to declare an international public health emergency (PHEIC), which lasted from July 2022 to May 2023.
That spike was driven by a new subtype, dubbed Clade II, which took over from Clade I.
Around 140 people died out of about 90,000 cases across 111 countries. That outbreak has now largely subsided.
HOW CAN MPOX BE DETECTED?
Countries are now able to detect cases, Rosamund Lewis, the WHO’s technical lead for mpox said, pointing to a system of surveillance, laboratories and communication with affected areas.
It is hard to know if there has been “a substantial rise” in cases, or whether “it’s just a matter of increased awareness”, said Maria Van Kerkhove, the WHO’s epidemic and pandemic preparedness and prevention director, who confirmed concern over the Clade Ib strain.

IS THERE A CURE, VACCINE FOR MONKEYPOX?
The recommended shot in Australia is the JYNNEOS vaccine, which was developed as a smallpox vaccine. For full protection, two doses are required at least 28 days apart. Two doses given before exposure to the virus is 84 per cent effective in preventing mpox and protection is believed to last for at least a couple of years.
Cases may still occur in people who are vaccinated, but these infections are typically milder. The vaccine is also effective after exposure to the virus, but less so than if it’s given beforehand.
On a more global scale, negotiations are underway between WHO and those countries affected by the Clade Ib strain about what vaccines can be licensed to help protect against the spread of mpox.
“There are some vaccines that are licensed that can be used for mpox,” Dr Lewis said.

WHO SHOULD GET VACCINATED?
Australian guidelines recommend vaccination in gay, bisexual, and other men who have sex with men. They also recommend vaccination for sex workers, and people with HIV who may be at risk of exposure to mpox.
Health-care workers who treat or are likely to treat patients with mpox are advised to consider having the vaccine.
Post-exposure vaccination is recommended for people who public health authorities classify as having had a high-risk mpox contact in the previous 14 days.
More Coverage
Read related topics:Explainers




