Radical technology that may transform Victorian healthcare
Pain-free motion and a solution to antibiotic resistance are just two of the groundbreaking medical projects under research by innovative Victorians.
Future Victoria
Don't miss out on the headlines from Future Victoria. Followed categories will be added to My News.
Victorians enduring debilitating conditions and lack of motion could soon be a step closer to walking pain-free again, thanks to innovative research into futuristic technology.
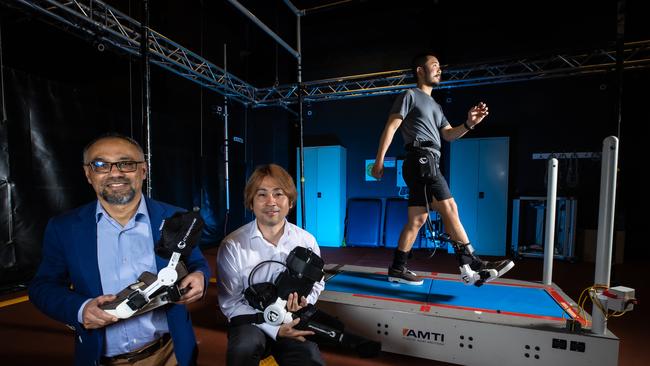
Researchers from Victoria University are developing a wearable device, small enough to fit on a shoe, which could reduce falls in disabled and older Australians.
Through biomechanics, robotics, computational intelligence and wearable senses, it’s hoped the technology will train the brain of those with neurological and musculoskeletal injuries as well as gait impairments to move the affected muscle freely.
The technology will also benefit those with chronic conditions such as diabetes, stroke and osteoarthritis.
Victoria University researcher and leader of the Program in Assistive Technology Innovation (PATI), Professor Rezaul Begg, says the device provides ankle joint assistance to help people with mobility difficulties walk more comfortably, while creating a “memory effect”.
“So a person sitting on a chair (for example), can use it to assist with lifting the foot and if used for some time, it will program the brain to lift their foot safely,” he told The Herald Sun.
While this research project will benefit Victorians enduring a lack of motion, it also advances the future of technology across the state’s healthcare system with the hope of replacing centuries-old walking aids and frames including wheelchairs and walking sticks.

Professor Begg said his team’s research is also opening up the door for successful international companies to share their technology with the state while boosting local hospitals.
The research project, titled Using Machine Learning to Optimise HAL Exoskeleton Joint Control, is in collaboration with Japanese partners CyberDyne and the University of Tsukuba.
The new device is a combination of CyberDyne’s world-first hybrid assistive limb (HAL) with Victoria University’s “smart” joint controls.
“(Victoria University) is the first in Australia to (collaborate) with (CyberDyne) at this stage, and now their focus is to come to the Australian market,” he said.
“We will also be collaborating with local hospitals, like Western Health … and the new hospital coming to Footscray, and we are thinking that this device could be part of their rehabilitation services.”
Professor Begg is a recipient of the Victorian government’s Veski Study Melbourne Research Program grant, which is funding the project, and it is hoped that by the end of this year there will be enough data to test the state-of-the-art device on a larger scale.
The Victorian University Professor said he is grateful for the support from his fellow students and researchers including research fellow Dr Hanatsu Nagano, CyberDyne’s CEO and president Professor Yoshiyuki Sankai, and Japanese falls prevention medical specialist Professor Katsuyoshi Mizukami.
Hopes grow for solution to antibiotic resistance
A Melbourne research team is hoping to deliver for worldwide use a solution to antibiotic resistance.
The loss of antibiotics, says Christopher McDevitt, is one of the major health issues of our time.
University of Melbourne’s Professor Christopher McDevitt is a laboratory head in the Doherty Institute where he is leading a team searching for ways to improve the use of frontline antibiotics to treat major infections such as pneumonia and sepsis. These are two of the leading causes of death in Australian hospitals.
But first his research team needs to attract around $2m in funding to get them across the line. Professor McDevitt said investment from government grants and philanthropic funding was urgently needed over the next five years so that his team could complete the necessary preclinical and clinical trials of their world-first therapy.
“Whenever we see a funding opportunity we go after it because we are passionate about moving this project along,” Professor McDevitt said. “Our society desperately needs solutions to the antibiotic resistance crisis, and I believe that rebooting already existing, readily available and cheap antibiotics is one of the quickest ways forward.”
Professor McDevitt said funding this work was an opportunity for Australia to make a global impact by 2030.

He was recently awarded a $100,000 Victorian Medical Research Acceleration Fund (VMRAF) grant to further his team’s work to make existing antibiotics, such as penicillin, effective weapons again against resistant bacteria.
He showed this was possible in a world first discovery this year where his team repurposed a molecule called PBT2 – which was originally developed as a potential treatment for disorders such as Alzheimer’s, Parkinson’s, and Huntington’s diseases. He showed that PBT2 could break bacterial resistance to commonly used frontline antibiotics in mouse models of infection and did not lead to further drug resistance.
“We knew from earlier studies that the immune system uses zinc as an innate antimicrobial to fight off infection,” he said at the time. “So, we developed our therapeutic approach with PBT2 to use the body’s antimicrobial zinc to break antibiotic resistance in the invading bacteria.
“This rendered the drug-resistant bacteria susceptible to frontline antibiotics, such as penicillin and ampicillin, and restored the effectiveness of the antibiotic treatment in infected animals.”
Resistance to antibiotics occurs, says the World Health Organisation (WHO), when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines. This makes infections harder to treat and increases the risk of disease spread, severe illness, and death.
The WHO has said that drug resistance is making antibiotics and other antimicrobial medicines ineffective such that infections are becoming increasingly difficult or impossible to treat.
“Australia has an opportunity to invest in developing therapeutics that can help both ourselves and the world,” Professor McDevitt said.
He leads a team of five postdoctoral researchers and nine students at the Doherty Institute in the heart of Parkville’s biomedical research precinct.

“We are trying to accelerate the research and deliver a new therapy,” Professor. McDevitt said. “More funding will allow us to conduct the preclinical studies and evaluate PBT2 in combination with two different, but commonly used, cost-effective antibiotics – amoxicillin and doxycycline.”
He said clinicians had told the team these were the two antibiotics they urgently wanted to “rescue”. They also wanted a treatment that was cost-effective and simple to prescribe for patients.
“Rather than prescribing two different antibiotics to try and avoid bacteria evolving resistance, our PBT2 combination therapy will allow clinicians to use a single, cheap antibiotic without resistance concerns,” Professor McDevitt said.
The team is focused on developing a therapy to treat pneumonia, but is also working on longer-term goals to develop PBT2 combination therapies to treat sepsis infections and ventilated associated pneumonia.
“Ventilated associated pneumonia doesn’t occur often in hospitals, but is very problematic. Once a patient gets infected the mortality rate is nearly 50 per cent,” he said.
Professor McDevitt said the team had applied to various funding bodies including asking for a $1m NHMRC Development grant that would allow them to do the preclinical work and pharmacology safety studies.
Although he does not yet know if they will receive the funding, he said it was critical to enable his team to conduct studies and ensure that the therapy would be safe and effective before moving into human clinical trials.
“Both the antibiotics and PBT2 have been tested individually in humans, so we already they are very safe. But we need to be sure the combinations are also safe and effective before clinical trials can proceed,” he said.
Professor McDevitt said a further $1m would be needed for a clinical trial in humans.
He is passionate about remaining in Australia to do the research, saying that while he has worked overseas, he came back because he wanted to return on the investment Australia had made in him.
“I believe I have a responsibility to contribute to how Australia addresses crucial health issues,” he said.
3-D printer for fabricated skin
It may sound like science fiction coupled with big dreams: creating biofabricated skin on a 3D-printer to repair lost or damaged skin in the treatment of burns, trauma and cancer patients. But the team behind a globally innovative research project being developed at the Aikenhead Centre for Medical Discovery (ACMD) are true believers.
They are determined to one day artificially create the core three layers of human skin and use them to make a novel synthetic tissue that can be blended with a patient’s own cells.
Led by St Vincent’s Hospital Melbourne and RMIT University, in collaboration with the University of Melbourne, their innovative technique may eventually produce bio fabricated skin that will avoid rejection, rapidly repair wounds and reduce scarring.
This is a team from diverse backgrounds: clinicians, dermatologists, scientists and PhD students working together in a rich environment where inquiring minds are encouraged to question and challenge to find answers.
Chris Baker is the director of Dermatology at St Vincent’s Hospital Melbourne jointly leading the project with Robert Kapsa, Professor of biofabrication and tissue engineering at RMIT University.
Associate Professor Baker admits it may surprise some that clinicians are working with engineers, but he says it is this working together on a problem that may have helped find the solution in artificial skin.

“I’ve been practising in clinical dermatology for 30 years,” Professor Baker said. “I have also been very involved in teaching and it was working at a place like St Vincent’s where you collaborate with other specialty streams doing clinical research that you identify what’s needed.”
Producing enough skin to repair a wound from surgery, burns or cancer treatment has long been issue for many surgical specialties.
“The long-term goal of this project is to make a material the patient recognises as their own; that will have greater acceptance,” he said. “If we can achieve this then bio fabricated skin may have use in a range of specialties including dermatology to plastic surgery and orthopaedics where we could need a material in quantity to repair loss or damage.”
In the collaborative environment of the ACMD, Professor Baker said the team had a light bulb moment.
“I was chatting to some colleagues in other specialties and one group was looking to produce cartilage (the strong, flexible connective tissue that protects joints and bones) and I thought if we are going to make bespoke human parts for patients it is going to need all the different components including skin,” he said.
The goal now, he said, was to produce a biofabricated skin that looks, feels and behaves as close as possible to a patient’s own skin but cautions the reality of bio fabricated skin is still some years away.
“What we hope is that biofabricated skin, when available, will improve the quality of life for patients with skin loss from trauma and chronic disease, with far more natural outcomes,” Professor Baker said.
Professor Kapsa said the team was working on tailor-making the three layers of skin to engineer a tissue that is more reflective of human skin than existing models.
“We hope this will translate to an artificial skin with more natural structure and function,” Professor Kapsa said.
Initial applications are also investigating if the material can be used to test medications and cosmetics including to develop surgical dressings to help speed up the healing process and to test topical drugs and cosmetics to gain realistic results without the need for using animal models.
“We hope ultimately to get to a stage where bio fabricated skin can be integrated with other engineered tissues such as muscle, nerves or bone to repair damaged limbs or other body structures – that’s just one of the potential long-term gains,” Professor Baker said.
He said while the reality of the bio fabricated skin was still some time in the future, every day gains were being made.
“And while it is always uncertain that you can develop something that can be applied clinically, we are climbing the mountain. We know where we want to get to.”




