The 1.5m myth: alarming distance Covid can travel and stay in the air
A Brisbane professor named one of the world’s most influential people by TIME Magazine says her honour has been clouded by the fact her dire Covid warning to the World Health Organisation was ignored for too long.
News
Don't miss out on the headlines from News. Followed categories will be added to My News.
As Lidia Morawska stirred awake, her resolve from the night before to act, to shake things up, escaped her momentarily.
“I remember thinking, ‘Do I really want to do this?’,” says Morawska.
“It had started growing on me, the hugeness of this undertaking. But my inner voice was telling me that I must do this.”
Her plan? To marshal eminent scientists from around the globe to pressure one of the world’s most influential groups, the World Health Organisation, to admit that it was wrong. Deadly wrong.

It was late March last year and the virus that causes Covid-19, SARS-CoV-2, was roving across the world and deaths were rising.
Concerned colleagues in China and Italy had been calling Morawska – a physicist and distinguished professor in atmospheric and earth sciences at QUT and one of the world’s foremost authorities on airborne particles and their effects on health – pleading for her help. They couldn’t get authorities in those badly affected countries to listen to the science.
She knew, they knew, that a virus such as SARS-CoV-2 was airborne, capable of hanging in the air for hours and travelling significant distance. They’d done the studies, seen the evidence.
But WHO and national health authorities everywhere were caught in what Morawska, 68, calls “medical dogma”; the long-held belief that viral particles could not travel further than arm’s length. Their advice for such a coronavirus remained as it had for decades; keep a distance of about 1.5m from others, wash your hands and sanitise surfaces.
It infuriated Morawska. “A complete misconception,” she says. But now, her frustration had turned to desperation. That weekend in March, WHO issued a communique, disseminated on Twitter, headlined: “Fact Check: Covid-19 is NOT airborne.”
“Well, this was something,” says Morawska. “It wasn’t disbelief, because I knew the medical community had this view but it was that alarm bells were rung. If WHO was spreading this kind of misinformation; this is wrong, this will lead to more cases.”
That Sunday, she wrote a letter to the WHO. That evening, she contacted colleagues.
Come Wednesday, March 31, she hit send on an email, signed by 36 scientists in fields such as physics, virology, engineering and medicine, urging change in WHO’s thinking – and directives. The virus, they said, could drift and survive in the air, especially in poorly ventilated and crowded indoor spaces.
Within an hour, Morawska had a reply from leaders at WHO headquarters in Geneva, setting up a Zoom meeting a couple of days later.

It didn’t go well. “When you know a group is against you – that was the feeling,” says Morawska.
It would take more than three months of lobbying and writing and badgering and advocacy by Morawska and her colleagues before WHO changed its advice.
Morawska’s dogged work led her to be named by TIME magazine as one of the world’s 100 most influential people for 2021.
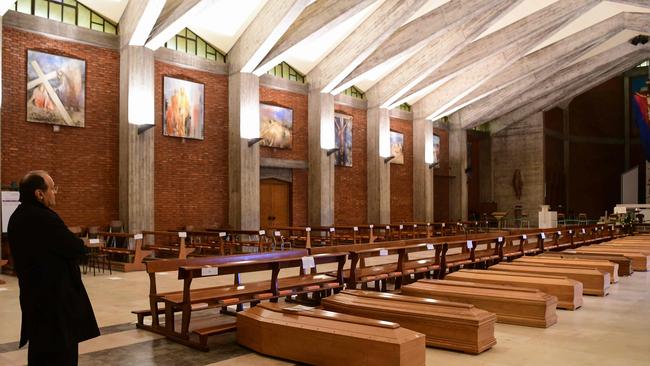
It’s an honour for all involved, she says, but clouded by the fact that the delay in WHO altering its advice, meant “we lost people. That’s the tragedy”. And there is still work to be done.
GOING NUCLEAR
Just why a bright 10-year-old girl growing upin the southeast Polish town of Przemysl in the 1960s set her sights on becoming a nuclear physicist escapes Morawska now. Perhaps it was an admiration of fellow Pole, Marie Sklodowska Curie, the physicist who pioneered work on radioactivity. Maybe it was Morawska’s love of nature and the fact that nuclear physics “goes into the very depths of nature”.

She went to university in Krakow and became interested in environmental radioactivity, leading to a PhD on radon, the naturally occurring radioactive gas that emits particles when it decays. The physics of airborne particles was luring Morawska.
In 1986, she relocated with her husband, Jan, and two daughters, Alina and Eliza, to Canada; first to the International Atomic Energy Agency at McMaster University, Hamilton, and then to the University of Toronto.
At Toronto, she had access to a coveted, hi-tech instrument that measured size distribution of ultrafine particles of just a few nanometres. Her curiosity took over.
“On some occasions,” she recalls, “I’d put a probe from the instrument outside the window on the ground floor in downtown Toronto. I saw so many particles. Huge. Tens of thousands, hundreds of thousands. Where did these particles come from?”
She looked through the literature. “There were basically no papers on this topic but it was, of course, to do with combustion and traffic and so on. I thought, ‘Wow, this is interesting and important’.”
She supercharged that interest after arriving at Brisbane’s Queensland University of Technology in 1991, forming what is now known as the International Laboratory for Air Quality and Health, a WHO collaborating centre, in 1992. It was a grim year personally; Jan died from melanoma. Morawska has since married Luis Ferreira, a professor in civil engineering, who she met at QUT when working on projects related to vehicle emissions.

It was in 2003 that Morawska became fascinated by the largely unexplored physics of airborne viruses, ironically after her expertise was sought by WHO. Would she go to Hong Kong to investigate the mystery of Amoy Gardens?
This was the scenario: more than 300 residents in this apartment complex had contracted the first severe acute respiratory virus, SARS-CoV-1. Epidemiologists had been unable to determine how. An infected man had spent one night there but the virus had spread to “people in different buildings, people who had no physical contact with him”.
The trip didn’t eventuate but the curious Morawska was hooked.
“I started looking into this topic because we are still talking about particles but the particles from our respiratory system,” Morawska says.
These particles can be produced by exhaling and talking, not just sneezing, coughing, shouting or singing.
“Before a person is infected, it is really about the physics of these particles: how are they generated, what happens to them in the air, how they are inhaled and where they deposit. From then, the clinical aspects start.”

Again, she looked at the research and again there was very little, just a few papers from about 60 years ago. Here was scope for exploration.
She applied for an Australian Research Council grant in 2005 and the ensuing paper is “considered quite fundamental in terms of our understanding of what is the size distribution, (which) in the first instance, determines where the particles go”.
“If the particles are very big, they won’t go anywhere, they’ll drop to the ground,” Morawska says. “If they are small, they can float into the air and we have shown that the vast majority are small; sufficiently small that they can float in the air and they can stay in the air for quite a long time.”
Indoor spaces with poor ventilation are particularly good places for viruses to hang around.
Morawska says the physics is undeniable, proven. But the medical world was still wedded to protocols established generations ago.
Protocols, says Morawska, that were based on incomplete science, and therefore, incorrect conclusions. The history of how this came to be is fascinating, filled with varying micro-measurements and definitions and fuelled by the sometimes silo-like nature of different scientific disciplines.

But in essence, says Morawska, the medical protocols were based on 1930s studies that looked at large viral droplets.
“These studies dealt with larger particles which showed that these particles don’t go further than arm’s length. That’s how the medical dogma was formed that if you are at arm’s length from an infected person, you are fine because everything drops after this. It is right, everything that is big falls to the ground,” she says.
“But that study didn’t deal with anything smaller. Considering only the big particles is not the complete picture. From the point of view of science … it was absolutely clear that the virus is in the air.”
This was the charged atmosphere that Morawska and co-signatories of the letter to the WHO dialled into in early April last year for the Zoom meeting with about 10 WHO officials.
One co-signatory, Dr Linsey Marr, an aerosol scientist at the US’s Virginia Tech, has told the technologies magazine Wired how aghast the team was when a WHO representative cut Morawska off, telling her she was wrong about how far infectious particles can travel. “You just don’t argue with Lidia about physics,” Marr said.

Morawska hung up with a heavy heart. “There was no real urgency, no real acceptance, no real evidence that they would do something about it.” It was about 11pm. She tried to sleep. She couldn’t. “I got up and drafted some things in response and what needed to be done.”
Some colleagues were clear; go to the mainstream media. Morawska held firm. Let’s not alienate or damage the WHO, she cautioned.
“I didn’t want to do harm to the WHO because it is an important organisation.” She was acutely aware that then US president, Donald Trump, was planning to pull funding from the WHO.
It was decided to send an article – signed by 239 scientists from an array of disciplines – to the well-regarded British science journal, Nature.
The article pointed to a range of studies about airborne transmission of viruses, argued that this was the only plausible explanation for a number of superspreading Covid-19 events and called for improved ventilation, particularly in public buildings, workplaces, schools, hospitals and aged care homes.
Nature took a few weeks to reply, “while the pandemic is raging”. The article was rejected. The feisty Morawska recalls telling the editor “what I thought about this”.

She sent it to The Lancet, one of the world’s oldest and most respected medical magazines. It was rejected again, with one reviewer concerned about repercussions if it was made public. “I said, ‘This is not review, this is censorship’.”
By now it’s early June, the wearing of masks is still not widely promoted, and talk of the importance of ventilation is muted. Thousands are dying. Correspondence with the WHO was continuing but leading nowhere. Says Morawska: “There was outrage in our group: ‘What are we going to do if we can’t get this message out?’.”
Someone had a contact at the US journal, Clinical Infectious Diseases. “Luckily this editor, a medical person, was open-minded, considered this was important and they said ‘Yes’.”
The article appeared on July 6, 2020. “It was a media storm, really, a media storm,” she says.
The next day, WHO acknowledged “new evidence” about airborne transmission of the virus. Morawska smiles wryly. “Well, ‘new evidence?’,” she chortles. Still, it was a win. On July 9, WHO published a scientific brief, acknowledging airborne transmission.

Morawska is pleased to have made a seminal difference in the understanding of the spread of Covid-19 but says the updated WHO brief is still not correct, because it emphasises transmission being “mainly” through close contact.
“Indeed, if you are very close to an infected person the concentration is the highest so a short exposure time will lead to much higher inhalation. But it doesn’t mean that on a population basis that most infections occur at a close distance,” Morawska says.
She points to the many cases where transmission is believed to have occurred in hotel quarantine, where close contact was minimal or non-existent. “Many big outbreaks were not because of close interaction. So that ‘mainly’ is not correct,” she says.
“The problem is, saying ‘mainly’ gives a way out for public authorities; if it is mainly spread this way, then they (can argue) they are targeting the main problem. Which means put physical distance. Solved.”
Not solved, Morawska says. Such qualifying words in the WHO statement need to go. And it’s time for a much more detailed conversation – and action – on ventilation in buildings.
CLEARING THE AIR
A light breeze wafts through the open window of Morawska’s small QUT office, her door is open and a device the size of a portable alarm clock sits on her desk. It’s a carbon dioxide monitor and she takes it everywhere, just as she does a mask, something Morawska was using indoors long before the rest of us.

When dining out, she places the monitor on the table. If the CO2 reading rises from a “fresh air” state of 400 parts per million to 800ppm and beyond, she asks to move outside.
“When the windows are closed and the airconditioning is on, the concentration of CO2 can be very high. You wouldn’t realise how many restaurants in Brisbane have basically no ventilation.”
CO2 builds up in poorly ventilated spaces and is easier to measure than virus particles, making the monitor’s readings a useful proxy for the risk of exposure to SARS-CoV-2.
Pre-Covid-19, an 800ppm level of CO2 might make you a bit sleepy. In our pandemic world, says Morawska, if a Covid-19 infected person was in the room, “the virus concentration could be such that people could be infected”.
Ventilation. It’s essential to living well with Covid-19, says Morawska. But getting meaningful action is hard. “If you mention to anybody about indoor air quality, (they think) ‘boring’,” she says.
At the very least, mechanical ventilation systems, such as supply and exhaust fans, and airconditioning systems and filters should be checked regularly for effectiveness. “Often buildings’ ventilation systems are not maintained properly,” she says. Windows are gold.
She’d like to see carbon dioxide monitors in multiple places in buildings.

Just what constitutes a “crowded” indoor space is not straightforward. During a recent visit to the Brisbane Planetarium, with scores of people, the CO2 level was safe, aided by the high dome and good ventilation.
But she says, if she closed the window and door on her small office now, the CO2 level, which has moved from 440 to 510ppm since my arrival, would be over 800. “A crowd of two,” she says.
Schools are a concern to Morawska, who says the reliance in hot months on airconditioners, which often recirculate air, is problematic. Recirculation is important to save energy but does not improve air quality and can lead to high CO2 levels which, even without the virus, can make students lethargic.
Air purifiers help filter out viruses, and she is supportive of the Victorian government’s move to roll out more than 51,000 air purifiers to the school system. She’d like similar action in Queensland, and is meeting with health officials. But purifiers are a stopgap measure that add to energy usage.
It’s like putting a bucket under a leaking roof, Morawska says. “It won’t be flooded but in the longer term, you have to fix the roof. In the pandemic, it’s okay to put the bucket in terms of an air purifier but in the longer term, this is not the solution.”

Better building design is, and that’s why enforceable changes to Australian standards are needed. Indoor air quality is given lip service in the standards, Morawska says.
There is a table about pollutant concentration but no requirement to measure the pollutants. “If it’s not measured, nothing is done. I’m still trying to get my head around why the table is there. For decoration?”
She says Queensland is well-placed to embrace indoor/outdoor design that prioritises airflow. Architects, designers and engineers want to incorporate such concepts but if it adds to cost, their ideas are often rejected.
“Ventilation is the last interest,” she says. “For a fistful of dollars, we risk ventilation.”
The pandemic has proven that’s a false economy, she says. “How much does the pandemic cost? How many times under normal circumstances are we sick from cold, flu? The medical costs of this; the lost productivity, absenteeism, all of these are costs, too.”

If the weight of legislation – and government – is behind advancing air quality as a priority, then innovative approaches will follow.
She envisages smart buildings that sense the number of people inside, dictating how much air needs to be brought in (through old and yet-to-be-discovered methods) to reduce carbon dioxide and other pollutants, viruses and bacteria.
“It’s all possible, it just takes the sensing technologies which exist and could be used; it takes data interface and data interpretation which would be quite complex but possible.”
It’s such possibilities that Morawska hopes being named as one of the world’s most influential people will help her advance. TIME splits the top 100 into subgroups, and Morawska comes under the “Innovators” banner, alongside SpaceX’s Elon Musk. She finds the grouping a little anomalous, because “I didn’t invent”.
But what she did was momentous. Morawska and her fellow scientists alerted the world to a serious fault and drove lifesaving changes.
Now, she’s keen to use her recognition to drive the world towards designing and embracing smarter, healthier buildings.
“The invention in all of this,” Morawska says, “is coming.”
More Coverage
The smart way to keep up to date with your Courier-Mail news
Originally published as The 1.5m myth: alarming distance Covid can travel and stay in the air




