St Vincent’s chemo scandal: Families’ desperate search for answers begins again
MICHAEL Tozer, a father-of-two, received chemotherapy from Dr John Grygiel at Daffodil Cottage in Bathurst. Now his family have been promised a case review.
NSW
Don't miss out on the headlines from NSW. Followed categories will be added to My News.
- SPIN DOCTORS PUT PATIENTS LAST DESPITE FEARS
- ST VINCENT’S HOSPITAL’S SICK CANCER SECRET
- FEARS THERE COULD BE HUNDREDS OF VICTIMS
FAMILIES of cancer victims treated by the doctor at the centre of the St Vincent’s underdosing scandal were yesterday demanding answers from authorities.
Michael Tozer’s family said the 47-year-old had “breezed through” chemotherapy for his oesophagus cancer but died in agony months later.
They were yesterday promised his care under Dr John Grygiel, who underdosed at least 78 head and neck cancer patients at St Vincent’s Hospital, will be reviewed.

The commitment from the Western NSW Health District came only after the family asked for his case to be examined.
It’s director of clinical governance, Di Wykes, said the facility had reached out to a “number of patients” who were treated by Dr Grygiel during his tenure as “honorary medical officer”.
Mr Tozer, a father-of-two, received chemotherapy from Dr Grygiel at Daffodil Cottage in Bathurst before undergoing radiation after he was diagnosed in February 2010.
“He breezed through the chemo,” his wife Sharon Tozer said.
“It makes me wonder whether he received the right dose because he said he was feeling great.”
In June they went for a second opinion but claimed they were told it was “too late” to operate and they should have come sooner.
Then, soon after, they received devastating news — Mr Tozer’s cancer had spread to his bones.
He continued to work up until the last six weeks of his life to provide for his family — his youngest daughter was only one.
“I don’t know if it would have made a difference but now I’m questioning it,” Ms Tozer said.
“I’ve been told his case will be reviewed since all of this came out. I need answers, I just want to know.”
Dr Grygiel is overseas but his lawyer yesterday denied he had underdosed patients, two months after the oncologist told The Daily Telegraph patients had “suffered no damage by the lower dose that was administered” and said people had done better “because they’ve had less side effects”.
His lawyer added: “Dr Grygiel needs to communicate with St Vincent’s Hospital before communicating with any of his former patients and he will do so on his return to Australia next week; that is he will discuss with St Vincent’s Hospital the possibility of communicating with former patients.”
Lisa McLean’s mother, Maria Tait, from Lithgow, was diagnosed with stage three ovarian cancer in 1999 and, after being initially treated at Westmead Hospital, Ms McLean says Dr Grygiel gave her carboplatin at Daffodil Cottage chemo unit in Bathurst.


She also had surgery and was treated with other drugs.
In 2001 Dr Grygiel told Ms Tait that the carboplatin “failed” and told her to go home and make the most of the rest of what was left of her life. However, Ms McLean claims no palliative care was organised for her mother.
“Mum went home and was there for about two months until it reached a tipping point where she couldn’t eat. No palliative care had been organised. She was basically a living skeleton on the lounge — not even any Panadol.”
Ms McLean, who lives in the Newcastle area, made formal complaints about Dr Grygiel’s treatment to her GP in Lithgow and a senior doctor at Westmead.
As her mother’s health deteriorated further she was rushed to Westmead Private Hospital where she received palliative care and painkillers. She died not long after, in 2001.
Ms McLean said she supported calls for a special commission of inquiry into Dr Grygiel’s treatment methods.
A spokesman for St Vincent’s last night said it could not provide “details on particular patients” because of “strict privacy rules”.
Debbie Bennett’s 60-year-old mother Margaret was treated by Dr Grygiel in 1997 and later sought a second opinion for the cancer which had spread and was terminal.


She had chemotherapy through Dr Grygiel in Orange along with radiation. There was no operation — something Ms Bennett, an aged care nurse, questioned and held concerns about at the time.
“I don’t know why they didn’t cut it out then from the word go,” she said.
“They thought they could get it from the radiation but it cause bad burns. He then said go home and come back in six weeks and decide what to do.”
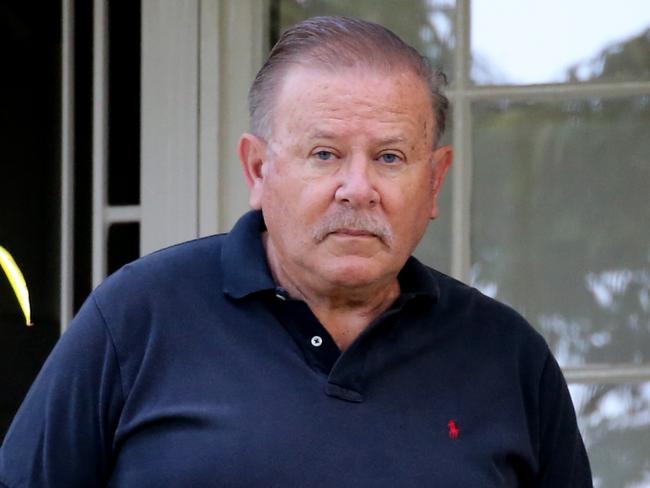
Public service worker Gary Kinkade, 54, was diagnosed with tonsil cancer in March last year.
He was treated by Dr Grygiel at Kinghorn Cancer Centre and after six months of treatment with Carboplatin and radiotherapy was put into remission.
The anxiety that grabbed hold of the Canberra man when he was first diagnosed has returned in the wake of the report into underdosing of some oncology patients at St Vincent’s Hospital.
“I am one of the lucky ones; I do feel good but it’s just that underlining thing in my head, now I have the anxiety again I’m worrying about the future again,” Mr Kinkade told The Telegraph.

The father of adult children said he had pleaded with St Vincent’s Hospital for tests to be conducted to confirm that he was cancer free upon finding out about the flat-dosing.
He said he had also pushed to be put in contact with the other patients affected by the underdosing so they could form a support group.
“Most of the information we are finding out about is from the media. I sit back here and think I’ve been in remission for nine months but it’s just that uncertainty now,” Mr Kinkade said.
“I feel alone and isolated, other than me taking it on myself to keep in contact with one other cancer patient — if it wasn’t for him and I — I would have no contact with anyone else, I feel like the hospital is keeping us all separate.”
STAFF TOLD THEY MUST STICK TO THE SCRIPT
Clarissa Bye
STAFF at St Vincent’s Hospital were given a set script to deliver to patients and their families when the scandal became public, including being told to say “the discrepancies have been found to have had no adverse impact”.
Secret internal emails show they were also ordered not to let distressed patients stay on the phone longer than 15 minutes.
“If patients have multiple questions suggest a follow-up phone call,” the instructions stated.
“Keep to the script if possible. Telephone conversations should only last 15 minutes maximum.”
After-hours nurses were told in a memo on February 19: “Please find below a script that after hours nurse managers are being asked to use over the weekend for any inquiries or distressed patients contacting the hospital in regards to the recent media issues.’’
They were instructed to say: “We understand that this might be a worrying time for you and may we reassure you we are aware that this matter is being fully investigated. The new prescribing system here at St Vincent’s was introduced in 2015 (and) has eliminated any chance of this occurring as all prescribing is done under strict guided protocols and calculations specific to each patient.”
A spokesman for the hospital last night said the phone calls were made in late February, when media reports broke about the issue: “We were trying to reach as many patients and their families as quickly as possible.
“We believed it would be less distressing for them to hear the information from us as opposed to the media. So the time frame we had to work under was tight.
“We were trying to reach as many patients as we could, as quickly as we could.
“Hence the reason for suggesting a follow-up call.
“One of the major aims of making these calls was also about assessing patient and family need — that is, what sort of support might a patient or family member need from us in the wake of this news?
“If they had a medical need, then we could arrange a follow up with a call from a clinician. If they were distressed and anxious, we could arrange for a follow-up call from one of our social workers.”
Originally published as St Vincent’s chemo scandal: Families’ desperate search for answers begins again




