GPs facing growing financial pressure to charge gap payments
A triple threat is brewing that will reduce your ability to see a bulk billing GP for a free consultation. Here’s why.

SA News
Don't miss out on the headlines from SA News. Followed categories will be added to My News.
A triple whammy looms for many people hoping for local GPs who bulk bill, with warnings it will add yet more pressure to the embattled public hospital system.
As the health system grapples with surging demand, experts have warned that gap-free GP appointments are becoming increasingly unsustainable.
A triple threat is brewing, including warnings that:
BULK billing is unsustainable for many clinics as Medicare rebates lag far behind the inflation rate, making gap payments inevitable in order to stay viable;
YOUNG doctors are shunning the pathway to become a GP, instead opting for other specialties with better pay; and
FEDERAL government changes which now make suburbs like Golden Grove and Belair priority areas for migrant GPs means overseas trained doctors are expected to abandon country towns to work off their 10-year bond and instead opt for suburbs.
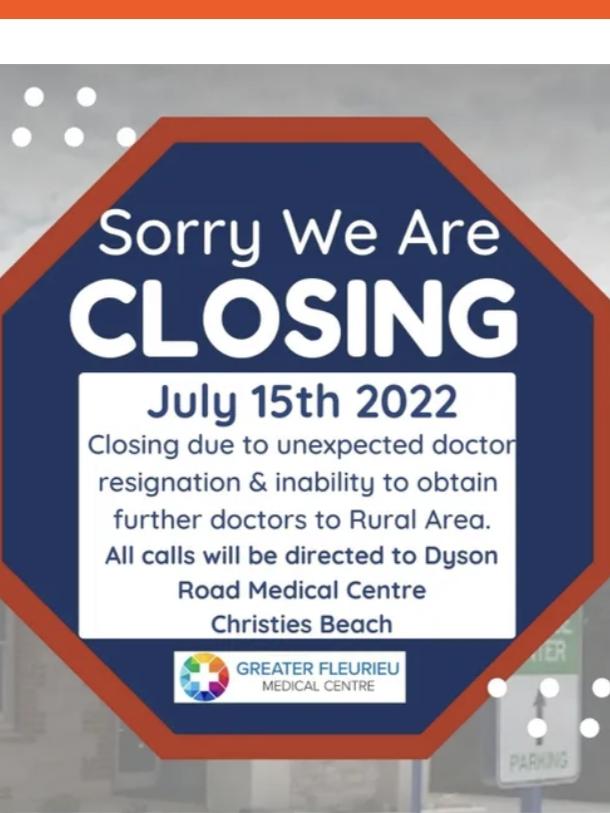
The Greater Fleurieu clinic at Yankalilla closed last month, citing an inability to attract doctors to rural areas, while this month Christies Beach Medical Centre dumped bulk billing including for pensioners who now face a $20 gap.

The clinic charges $80 for a standard consultation and $120 for a long consultation – the Medicare rebates are $39.75 or $76.95 respectively, leaving a gap fee of $40.25 or $43.05 for patients without a concession card.
Rural Doctors Association of Australia (RDAA) president Dr Megan Belot said country medical practices were seeing resignations as immigrant doctors “begin their migration to larger centres”.
“Many rural and remote towns will be abandoned by doctors who will move to more sociable, convenient and connected locations,” she said.
A combined shortage of GPs and a shift to charge a gap fee is forecast to see a rise in people heading to hospital emergency departments for “free” care for even minor problems.
RDAA state chair Dr Peter Rischbieth is concerned a lack of rural GPs will see people ignore relatively minor problems until they become an emergency, or not be given preventive care, again adding to ED queues.

The Australian Medical Association has joined the Royal Australian College of GPs in calling for an overhaul of Medicare amid a looming shortage of GPs as baby boomer doctors head for retirement.
The AMA says the freeze on Medicare rebates means the rebate covers less than half the cost of running a consultation.
The call comes as South Australia failed to fill its intake for GP registrars, with just 70 applications for the 110 places across the state this year with vacancies left for city and rural placings. Nationally, applications dropped from 2301 in eight years ago to 1329 in 2020.
The AMA estimates only 15 per cent of graduating medical students are interested in a career as a GP.
Young doctors are looking to other specialties – general practice is a specialty with first-year medical students facing a decade of training and exams before being allowed to register, then faced with the cost of running a small business.
Royal Australian College of GPs SA & NT chairman Dr Daniel Byrne noted other young doctors may prefer to stay in the public hospital system with its holiday pay, sick leave and pay rises well in excess of Medicare rebate rises.
“The past decade of inadequate Medicare rebate increases plus the freeze and then the more recent cuts to bulk billing incentives has led to this inevitable decision by general practices to charge private fees,” Dr Byrne said.
“Quality care takes times and time equals money. The majority of GPs do not want to compromise the quality and time given to patients so they need to charge a fee to cover essential business costs.
“Rapid throughput medicine is not acceptable to the RACGP and our members. The government wanted to push us to the brink putting the treasury department ahead of quality care. This is what happens when we put quality first - we charge a gap.
“The politics is messy. Why does private health get CPI increases or above every year? Now the shoe is on the other foot and it is time primary care was funded equally with all the other parts of the health system.”
Prime Minister Anthony Albanese has pledged to create a “strengthening Medicare fund” of $250m a year over three years from 2023-24 to make it cheaper to see a GP.
The rural GP shortage now sees locums being paid up to $3000 a day.
Originally published as GPs facing growing financial pressure to charge gap payments