Children’s lives on the line as health crisis deepens in the bush
Country children suffering bronchitis and tonsillitis are being flown to city hospitals at a cost of thousands because local health facilities can’t supply a $20 antibiotic to treat them.
National
Don't miss out on the headlines from National. Followed categories will be added to My News.
EXCLUSIVE: Country children with bronchitis and tonsillitis are being flown to hospital at a cost of $8,500 because local health facilities can’t supply a $20 antibiotic amid a deepening bush crisis.
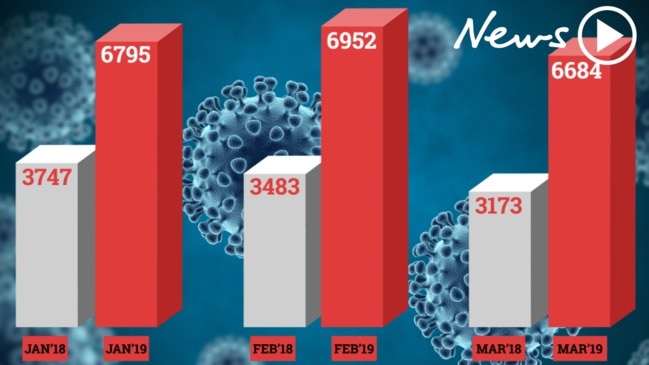
Figures show the Royal Flying Doctor Service has recorded a 60 per cent increase in aeromedical retrievals of children in the last four years as health services in the bush recede.
Between July 2014 and June last year, the RFDS conducted 13,026 aeromedical retrievals of children aged up to 14 years-old from remote and rural areas, RFDS CEO Martin Laverty said.
The main reason for air retrieval of children was respiratory illnesses, with bronchiolitis, pneumonia, and respiratory tract infections the top three, he said.
“This sort of stuff does not require an ambulance in the city, when it’s spotted early it can be managed by an antibiotic script,” Mr Laverty said.
But in bush towns without a doctor — and where there is no 24 hour medical coverage — children have to wait to access health care and become sicker until it becomes so acute the decision has to be made to fly them out, he said.
“An antibiotic script would cost around $20 but it costs $8,500 each time we deploy our aircraft,” he said.
Once they get to a hospital, children from the bush stay two and a half times as long as city-based patients while the average hospital admission costs $5,500, he said.

News Corp is campaigning to force both major parties to commit more funding to properly resource health services in the bush this election campaign.
READ MORE:
Shock waiting lists at hospitals revealed
Shorten accused of funding ‘merry-go-round’
The Rural Doctors Association has revealed a $2 billion a year underspend on health funding and health service delivery in the bush.
People in the country get 12.6 million fewer health services a year funded by Medicare than people in the city, the association said.
It means they are sicker when they do get treated and end up being admitted to hospital.
An extra $830 million a year is spent on acute hospital care for people from rural and remote areas compared to city people.
The National Rural Health Alliance is asking people to think about rural health when they vote and have released an election manifesto asking for help with four key priority areas.
These include government funding for 3,000 extra allied health workers in the bush including physiotherapists, dentists and mental health workers at a cost of $300 million.
They want a $400 million community grant fund to allow bespoke solutions to regional mobile phone black spots that make it easier to deliver telehealth.
They want Medicare to fund telehealth consultations for GPs in the bush.
Alliance chief Mark Diamond said more than $360 million in grants from the government’s Medical Research Future Fund should to go to rural health projects, an amount equivalent to the one quarter of the population that lives in the bush.
An extra 3,000 Aboriginal health workers at a cost of $180 million a year is also needed.
HEALTH DANGERS OF THE BUSH
Tonsillitis can easily be treated with antibiotics but it quickly became dangerous for five-year old Sophia Nicholls because of poor health resources in the bush.
Three years ago, living with her family in the outback town of Bourke, her airways were in danger of closing because of a severe bout of tonsillitis.
“The hospital told us they didn’t have the services to manage if her airways closed,” said her mother Kirsten Nicholls.

The Royal Flying Doctor Service was called to rescue the toddler who had to be flown to Dubbo Hospital for proper care.
“I shudder to think how much towns like Bourke are reliant on the Royal Flying Doctor Service,” said Mrs Nicholls.
“If we had tried to drive it would have taken four hours to get to Dubbo and it was too dangerous with her airways in that state,” she said.
“People in the city don’t realise what it is like in the bush unless they live there,” she said.
Mrs Nichols said Bourke Hospital was a great hospital but the town needed more specialists to visit on a regular basis.

Four year old Cruz Prior was on an extended family road trip through outback Australia when a fever struck and he was unable to access the life saving care he needed in a country hospital.
The Priors had sold their home in Melbourne and bought a caravan so they could travel up the east coast of Australia for six months with their three children.
Their youngest son Cruz had been battling leukaemia since he was just 16 months old and was still receiving treatment throughout the trip.
His mother Kelly Kajewski had carefully planned the journey with her son’s doctors.
“Anyone that has got something that compromises their immune system needs antibiotics quickly,” Ms Kajewski said.
“We took the rules very seriously and always made sure there was a hospital with an emergency department near where we were staying and there was mobile coverage,” she said.
But the best laid plans came unstuck when the city dwellers came face-to-face with the inadequacies of Australia’s rural health system.
While the family was staying in Lightning Ridge, a town with a hospital emergency department and mobile coverage Cruz developed a fever.
They took him to the hospital at 1.30am only to discover that the hospital had no capacity to carry out a rapid blood test to determine what was causing Cruz’ infection or the equipment to deliver IV antibiotics to a child.

Any blood tests needed to be sent to a hospital in another town and would not have been returned until 5pm the next day.
It was at this point the Royal Flying Doctor Service was called in to transport Cruz to Dubbo Hospital.
Mrs Kajewski has nothing but praise for the hospital staff who did the best they could with the doctor staying overnight with her son until the RFDS plan arrived.
“Before this happened I had no comprehension of what the Flying Doctor Service was, except for the TV show.
“It makes you realise that it’s so difficult to get access to healthcare in the outback,” she said.
TIME FOR A CHANGE
News Corp is campaigning for these changes:
• Federal government funding for fly-in fly-out GPs in towns that can’t attract a doctor.
• $72 million a year in federal funding for 500 fly in fly out allied health workers like dentists, physiotherapists and mental health workers for the bush.
• Federal funding for salaried GPs in small towns where Medicare funding is too small to make a living.
• Expanded Medicare funding for telehealth to cover GP consultations in the bush at a cost of $180m a year.
• Employ trainee country GPs on a salary and give them maternity leave and count their service towards long service leave while they train as GPs.
• Implement all recommendations of the 2018 Senate Inquiry into accessibility and quality of mental health services in rural and remote Australia.
• Reform GP the rural incentive payment of up to $60,000 to reward doctors who provide greater scope of service such as after hours and advanced skills.
• Introduce a rural loading for specialists to incentivise them to provide services in the bush.

