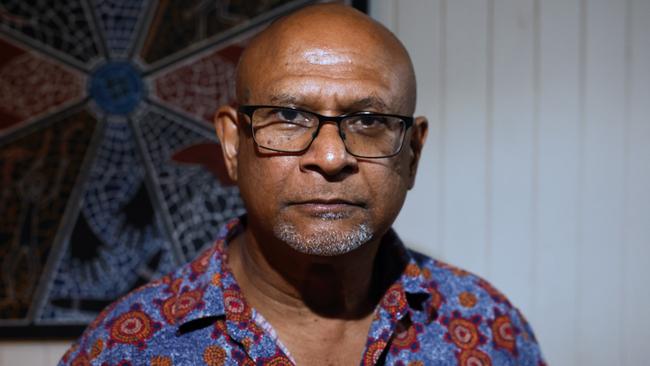
Dr Mark Wenitong talks about the high incidence of suicide among Indigenous youth and how it can be addressed
A prominent figure in Aboriginal healthcare has called out grave shortcomings in the health system, as data reveals Indigenous youth are taking their own lives at a rate three times higher than non-Indigenous youth.
Cairns
Don't miss out on the headlines from Cairns. Followed categories will be added to My News.
Indigenous children and teenagers are taking their own lives at a rate three times higher than non-Indigenous youth, data shows, with a stalwart of the Aboriginal health sector calling attention to alarming suicide rates in Indigenous communities.
According to the Suicide in Queensland Annual Report 2022, by the Australian Institute for Suicide Research and Prevention (AISRAP), Aboriginal and Torres Strait Islander youth aged under 20 accounted for 15.8 per cent of all suspected suicides by Aboriginal and Torres Strait Islander peoples in 2021, compared to 4.9 per cent for non-Indigenous youth who were the same age.
Dr Mark Wenitong, who holds a number of portfolios including co-chair of the Queensland Health Aboriginal and Torres Strait Clinical Network and advising commissioner on National Mental Health Commission, shed light on the prevalence of mental health problems in First Nations communities as everything from “mild issues” right through to suicidality or psychosis.
“Both those ends of the spectrum occur in our communities and the biggest background noise telling us something’s wrong is the suicide rates,” he said.
“We do have very high suicide rates in our community, particularly exaggerated in younger people, we’re talking very young – ten year olds – in places like the Kimberly.”
The impact on very young people was a serious worry, he said, due to their inability to actively seek help.
Some part of it, in his opinion, was a fallout of colonisation, resulting in fragmented identity and a lack of meaningful connection to modern day ideals and expectations.
But what was more concerning to him were the inadequacies in the health system when it came to following up after an attempt of suicide.

“People with suicidal intent who have ended up in emergency wards in Queensland are much less likely to be followed up from healthcare after a suicide attempt and they are classically red light high risk patients,” he said.
“Young people with psychosis, drug and alcohol psychosis, with failing to cope and mental health crises – all of those are overrepresented in emergency ward presentations but we are not red lighting them when they have to be followed up systematically, so the system isn’t working anywhere near as well as it should work.
In remote areas, the issues were lack of infrastructure and adequate resourcing with particular difficulty in accessing early childhood programs and social support, he said, which was of concern due to mental health issues largely stemming from unstable family environments.
According to the interim Queensland suicide register, regions classed as “very remote”, which included Bamaga and Weipa, had the highest suspected suicide rates at 27.4 persons per 100,000 people.
Torres and Cape health services reported the highest age standardised suspected suicide rates at 30.4 persons per 100,000 people, almost three times higher than figures in metros north and south which are 12.9 and 12.2 respectively.
Cairns and Hinterland recorded 20.9 persons per 100,000 with one of the highest male suspected suicide rates.
Dr Wenitong referred to research done in North Queensland looking at the cortisol stress response of First Nations university students, revealing a flattened cortisol response.
“And that’s not uncommon in other colonised First Nations communities,” he said.
“What the neuropsychiatrists tell us is that it is related to activated fight and flight continually from birth – high stress response to everything environmentally.
“Only in some families can you be in a war zone but get out of the trauma, come to somewhere else and start to heal.”
Primordial prevention – prevention of risk factors – deserved more focus, he said, as chronic issues like obesity, type two diabetes and drug and alcohol issues, had similar pathophysiology of low grade inflammation, which can come from a stress response related to stressors on the person.
“Unsafe neighbourhood, not having a job, poor relationships – all those things progress chronic disease,” he said.
“If you’ve been exposed to domestic violence, neglect or abuse in childhood, there is a much higher risk of chronic disease, mental health issues, suicide and substance abuse.”
The early childhood approach of ensuring kids and their families were supported to have safe, loving, environments with help in place to tackle addiction or DV issues was a crucial first step in eliminating the root of mental health issues, he said.
Protective cultural practices and strong pro social relationships were vital in strengthening families, with attention towards antenatal care “in a big way” being of utmost importance.
“For long-term overall chronic disease and mortality, we do have to start earlier than trying to intervene in early middle age,” he said.
Help seeking avenues are provided to empower vulnerable readers to reach out if they need assistance:
Lifeline: 13 11 14, lifeline.org.au
13Yarn Aboriginal and Torres Strait Islander Crisis Support: 13 92 76, 13yarn.org.au
Wellmob: wellmob.org.au
More Coverage
Originally published as Dr Mark Wenitong talks about the high incidence of suicide among Indigenous youth and how it can be addressed




