Artificial Intelligence will predict your chances of having a fatal cardiac arrest in the future
Artificial intelligence predicted sudden cardiac death risk with more accuracy than a doctor. Aussie doctors reveal what it could mean.
VWeekend
Don't miss out on the headlines from VWeekend. Followed categories will be added to My News.
Would you trust an artificial intelligence algorithm to predict if – and when – you could die of cardiac arrest?
For Johns Hopkins University professor of biomedical engineering and medicine Natalia Trayanova this isn’t a far flung dream.
She co-authored a groundbreaking study on how deep learning, a type of artificial intelligence, can predict a patient’s risk of sudden cardiac death (SCD) from arrhythmia, an irregular heartbeat, over the next decade.
Sudden cardiac arrest kills thousands of Australians each year – often without warning – and has an extremely low survival rate of about 10 per cent.
Dr Trayanova, who will be in Melbourne this week to share her work, said artificial intelligence (AI) could learn patterns from data that were hidden to the human eye.
“(One can) train the algorithm to find patterns that are predictive of some outcome,” she said. “We said, we want to predict the risk of SCD, find patterns in the data that are predictive of that.”
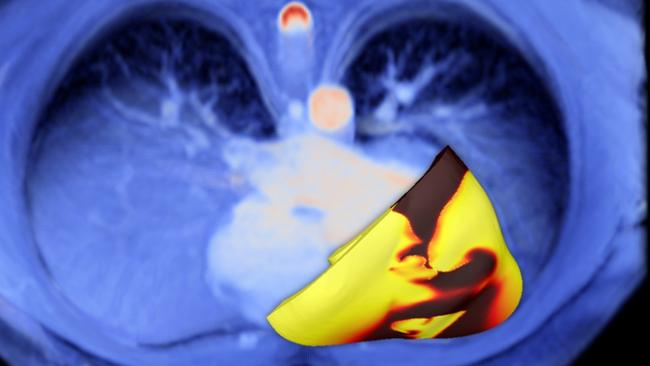
The algorithm learned to read raw MRI images of the hearts of ischaemic heart disease patients, analysing scarring patterns.
The world-first study was published in Nature Cardiovascular Research and found their deep learning tool – which she says now takes about 30 seconds to run – was more accurate than a doctor.
“The deep learning network … was able to predict from these images which patient is at risk for SCD, at what time in the next 10 years,” she said.
The current guidelines focus on how much blood a patient’s heart pumps out every beat but Trayanova said this only identifies 20 per cent of future SCD victims, meaning most miss out on lifesaving surgery to implant a special defibrillator.
“Many people will die in the prime of their life because the clinical criteria did not represent what was happening with their heart, so they remain unprotected,” she said.
But, she added, the guidelines also led to some patients undergoing an operation for a defibrillator they didn't actually need.
“A shock from a defibrillator is like a horse kicking you in the chest, it’s extremely unpleasant,” she said.
“Those are life-altering experiences.”
Her work has captured the public’s attention, but to Trayanova, the study was a natural step from her “twin hearts”.
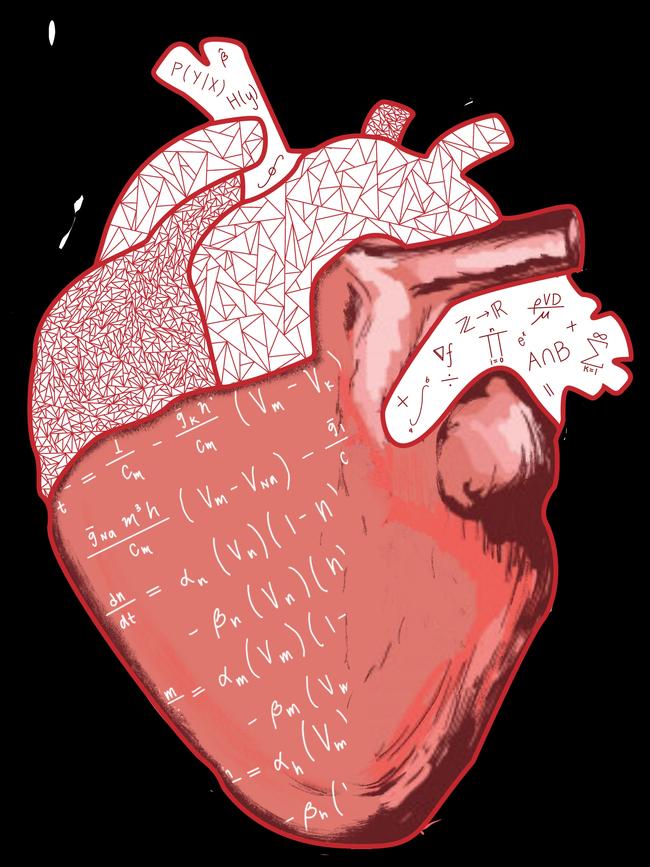
She is known in the research world for her work creating virtual hearts, a digital replica of a patient’s heart – built from MRI scans – that allows physicians to test treatments.
Despite the use of cutting edge technology, the individual patient remains at the core of Trayanova’s work.
This field, known as precision medicine, seeks to use all the new information we can gather about a patient to find the best treatment for that specific individual, as opposed to the best overall treatment for a population.
“It’s all very patient specific, which makes it very different from approaches that are one size fits all,” Trayanova said.
“(In the AI SCD study) we generate a personalised probability curve for each patient.”
Precision medicine also has a strong focus on proactive care, and seeks to identify issues months or even years before they arise.
Her SCD risk algorithm could one day help thousands more receive preventive treatment years in advance and shift the focus away from reactive care – which often comes too late.
So how will AI transform healthcare and precision medicine?
Trayanova said she envisioned a “really bright future” where AI analysed everything from other cardiac diseases to Covid and cancer.
“The machine learning tools … can be broadened, they can repurposed,” she said.
The key to AI’s future, she said, was to ensure we developed ethical AI, and life and death decisions are not based on data that only represents a portion of the population.
She said it was hard to say how long it will be until tools such as hers were available for clinical use and it depended on “institutional commitment”.
But she pointed to America’s Mayo Clinic, where clinicians already use AI to analyse recordings of the heart’s electrical activity, to prove it could move beyond the laboratory.
“When a clinician opens a patient record, there is a little button that he can click and say, ‘analyse the ECG of this patient’, and he sees it right away,” she said.

“To be part of clinical practice, it needs to become part of the infrastructure in the hospital.”
Regardless of how near or far that future is, there is one thing she is certain of: her tool is designed to assist doctors, not replace them.
“AI will never substitute clinicians, but I believe clinicians who use AI will substitute clinicians who do not use AI,” she said.
One clinician who isn’t afraid of AI’s potential, is Western Health’s cardiology director associate professor Nicholas Cox.
He said he was hopeful tools such as Trayanova’s could help save more patients from preventable deaths.
“There is nothing more saddening than when a patient who you’ve looked after for many years, and after following existing guidelines and rules, they end up having a tragic event, which perhaps if we had a more nuanced approach could have been averted,” Cox said.
He points to a decision he has to make regularly – whether to recommend implanting a defibrillator – and said AI could consider more nuances than current guidelines, which tended to have “a binary cut off”.
“We all accept that there must be a better way, even than three or four experienced cardiologists discussing it,” he said.
He said AI’s potential could even extend to data captured by patients’ phones, watches and fitness trackers.
“There are many instances, particularly in my field of cardiology, where there’s a huge amount of data being accumulated, and we just don’t know what to do with it.”
Cox acknowledges some doctors may feel unsure of artificial intelligence – describing it as a “black box” – but hopes it can prove its worth as research continues.
“I think it will help us make smarter decisions, have a more tailored approach to care for each individual patient,” he said.
Professor Graeme Clark knows all about scientific ideas that sound almost too good to be true. So it’s only natural that Trayanova has been invited to share her work at his namesake event, the Bionics Institute 2022 Graeme Clark Oration.
Clark has been recognised around the world for inventing the first bionic ear, which enabled deaf people to understand spoken language, but the Australian scientist says many at the time doubted him.
“When I started, 95 per cent of the public said it would not work,” he said.
“They went to the University of Melbourne even and asked for me to be dismissed, because it was seen as impossible.”
He said he ducked into another laboratory and “burst into tears of joy” when their first operation on a deaf man called Rod Saunders was successful in 1978.
He now believes AI is one of the new frontiers emerging in medicine and surgery.
“We’re at the cutting edge of a new, shall I call it, biomedical engineering era,” he said.
“Professor Trayanova’s work is very outstanding. It’s very easy to see that this is really, really soon likely to give benefits.”
But how does one convince the public – and patients – to put their health in the hands of new technology?
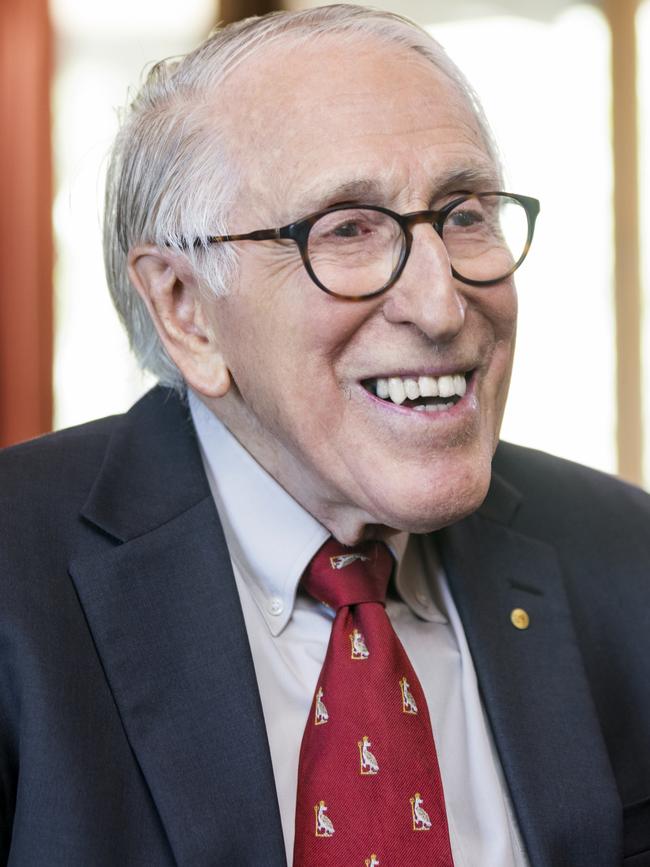
It’s a challenge Clark is familiar with, and whether it’s the cochlear implant or AI, he said the same principles applied: good research, ethics and communication.
“It’s very important to make sure that it’s done ethically and the patient knows what you’re doing, and needs to have it explained all the time,” he said.
He argues more funding is needed for Australians to fully unlock the potential of artificial intelligence in our healthcare system.
“I would like to see more money put towards fundamental research, because the two must go together. You’ve got to have the basic research,” he said.
“Australia does cut above its weight … but it’s got the potential to be a leader in biomedical engineering and medicine generally.”



