Migraines are destroying Australians’ lives and turn you into a ‘ghost’
THREE million Australians, mainly mums, are missing out on vital help for migraines which have emerged as Australia’s most neglected chronic illness.
Illness
Don't miss out on the headlines from Illness. Followed categories will be added to My News.
SPECIAL INVESTIGATION
A HIDDEN illness destroying the lives of millions of Australians, mainly mums, is being denied research funding and is being ignored by the medical profession.
Three million Australians are missing out on vital medical help for migraines which have emerged as Australia’s most neglected chronic illness.
The crippling neurological condition which causes paralysis, pain, vomiting, speech and vision problems is the third most debilitating medical condition in the world according to the World Health Organisation.
The degree of disability associated with migraines, which can last for days, has been found comparable to conditions like dementia, quadriplegia and psychosis.
Women are three times more likely than men to suffer the condition.
Yet in Australia only one per cent of sufferers are getting access to migraine specific medication.
Australian migraine researcher Professor Lyn Griffiths laments that vitamin company Blackmores has refused to develop her new vitamin combination that prevents migraines in some people.
“I’m keen to talk to someone who could partner with us to develop this,” she says.
This combination involves 2mg of folic acid, 25mg of vitamin B6 and 400mg of vitamin B12. Professor Griffiths cautioned seeing your doctor being taking the combination as it exceeds the recommended daily intake.

However, Dr Lesley Braun, the Director of Blackmores Institute, said: “The product does not feature in our range because the dose shown to be effective in the trial was four times higher than we would be able to include in our product because of regulatory restrictions.”
GPs are also unaware of Professor Paul Martin’s psychological treatments that have shown in clinical trials to reduce migraine by 77 per cent.
Professor Martin, from Griffith University in Queensland, has had success with his Cognitive Behavioural Therapy.
This involves identifying migraine triggers, changing a person’s lifestyle to avoid some triggers but exposing them to other triggers in a controlled way to reduce their ability to provoke a migraine, randomised controlled trials found it delivered a 77 per cent reduction in migraines.
Professor Martin says he was derided at an international neurological conference when he tried to explain to doctors that his methods worked.
“It leaves pharmacueitcals for dead, they prevent 27 per cent of headaches compared to our 77 per cent,” he said.
Headache Australia says there are no clinical guidelines for treating migraine in Australia.
There is only one doctor for every 100,000 patients and the chances of being correctly diagnosed is only one in 20.
In six years of medical training just four hours are devoted to headache.
Thousands of Australians have become addicted to pain and migraine medication because of poor understanding of the disease by doctors and bad management.
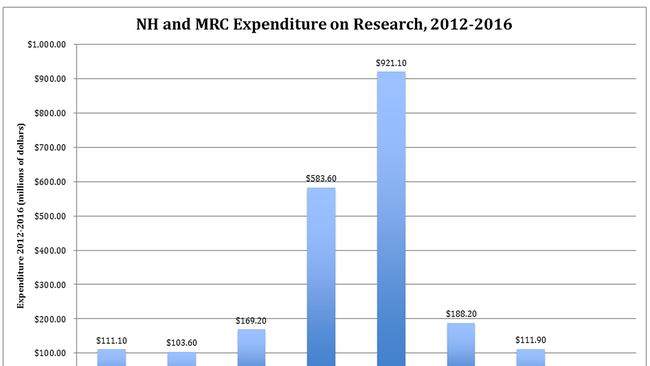
The National Health and Medical Research Council has allocated a paltry $2.6 million to research in the area in the last five years, this compares to $91 million spent on drug addiction.
The council recently knocked back an application for $2.5 million grant to set up a national centre for excellence into the condition even though Australia is home to world leading migraine experts.
Professor Martin says headaches cost the economy $1 billion a year and are responsible for 20 per cent of all working days lost.
“Migraines strike the young and middle aged, people who are driving the economy and doing all the work, they are at the stage where they are active contributors to society,” he says.
Today we start a campaign to get this disease the attention it deserves:
• The government should fund provide $2.5 million for a research centre of excellence in migraine to educate doctors about the latest treatments;
• Migraine should be made an NHMRC research priority area;
• Clinical guidelines should be written to reflect the latest Australian psychological and genetic research on the best treatment;
• All Australians with migraine should register with Headache Australia so politicians and pharmaceutical companies the size of the problem.
Headache Australia’s General Secretary Gerald Edmunds is urging headache sufferers to register with Headache Australia.
“Our major tactic is we want people to join the national headache register at the moment we have 10,000 but if we can get to one million we can exert political pressure for more research and new treatments,” he said.
A recent Migraine World Summit organised by Carl Cincinnato had over 60,000 participants from 158 countries who heard online talks from 36 experts, specialists, professors, neurologists, geneticists, authors and doctors.
‘IT’S DEVASTATING’
RACHEL Weston’s migraines were so bad before she started using Botox therapy she had only a few hours per month without pain.
The Melbourne mum, 30, suffered two to three severe migraines per week with mild to severe headaches on other days.
Not only did migraines mean she missed out on birthday and Christmas parties, other social events and work it’s even meant she had to give up plans for a second child.
“My migraines were the worst I’ve experienced during my pregnancy with my daughter Jazmyn (now 6 years old); I was greatly affected by migraine for a large portion of my pregnancy due to migraines, usually 3-4 days per week, especially in the third trimester,” she said.
“I wasn’t able to take any preventive or acute medications during pregnancy, and as migraines can be greatly influenced by hormones, I don’t think I could go back to having no treatment and being in constant pain again.”
Rachel tried Sandomigran, beta blockers, Topamax, antispasmodics, aspirin and nurofen and triptans to control her migraines but nothing worked.

She has received a new lease of life after starting Botox treatment for her migraines.
“I went from only having a few hours per month without pain to sometimes going up to a couple weeks at a time without head pain,” she said.
Her treatment sessions involve 32 Botox injections in her face, head, neck and shoulders every three months.
“You have to have 15 migraines per month to get the treatment,” she said.
Her mother gets migraines and her six-year-old daughter Jazmyn experienced her first migraine at age 4.
“It’s devastating, it’s the one thing I didn’t want to pass on to her”.
Rachel says migraines feel like a screw driver in your head.
“I feel nauseous but its rare I vomit, I lose co-ordination and I wouldn’t be able to walk,” she said.

“It’s definitely affected my career, when you have to take so much time off you are looked down on and it can affect your career progression.”
Rachel says the side effects of prevention treatments are not pleasant.
“I put on 15 kilos on sandomigran, developed pins and needles after Topamax, had dizzy spells and is was not safe for me to drive a car,” she said.
The Melbourne mum tried elimination diets, had multiple brain scans.
“How can you treat something when you don’t know what’s causing it,” she said.
Unfortunately the Botox treatment that has got her migraines under control is not proven to be safe during pregnancy.
“I basically have to choose between having another child or being relatively pain-free,” she said.
‘I’M THE FAMILY GHOST’
EMILY Lawrence Gazal says migraines make her feel like the “family ghost”.
“Instead of being the heart of the home I’m watching from the outside, I’m like a ghost, I’m there but I have to miss things like picking up and dropping off at school and making dinner because I’m too sick,” said Sydney mum and freelance writer Emily Lawrence-Gazal.
Emily, 44 from Bondi, says she has a headache most days and often has really bad ones that leave her bedridden for three days.
She’s tried multiple medications, prevention medicine, vitamin supplements, dietary changes and exercise to control the condition to no avail.
“The fact that all the painkillers are addictive and cause more headaches is pretty bad,” she said.
She’s terrified the treatments she’s taken have damaged her brain and is distraught that two of her young children have also developed migraines.
“GPs know nothing about it,” she said.
“You don’t talk about it, the pain doesn’t go away but people don’t want to hear you complaining about pain year after year.

“I’m terrified for my kids, the things they won’t be able to do in life because of migraines.
“My mum had them too and all the medications they have there is a problem with all of them, the more you take them the more likely you are to get the headaches.
“Five years ago a neurologist turned me away, he said he’d tried everything on me and nothing had worked. It was devastating.”
Carl Cincinnato who has set up Migrainepal, an app that helps people manage their migraines, suffered severe migraine for seven years says it’s a “perfectly evil disease”.
“On the one hand you’ve got the pain and suffering, nausea and light sensitivity and touch sensitivity, on the other side is the psychological torment, it’s a disease that keeps you on the edge, its out of control, you never know when the next one will arrive,” he said.
“It’s like being in a dark room, trying to find an exit and someone is in the room with a baseball bat waiting to hit you.
“Its an invisible illness, society doesn’t see it and you don’t get sympathy.
“Last year I had a person who had cancer and migraine and she said migraine was the more difficult because you got more support for cancer, but with migraine everyone turned the other way.”
Although millions of Australians suffer serious disability and miss work and social events because of migraine many never receive a proper diagnosis.
Nearly one in five women and one in 15 men suffer from migraine and one in three sufferers have to miss a day of work every three months.
Half of all migraine sufferers say their productivity when at work is reduced by 50 per cent because of migraine.

Different types of migraines.
1.Familial hemiplegic migraines are migraines with aura, provoke paralysis down one side of the body and they are linked to neurotransmitter genes. A genetic test is available.
2.Vascular migraines are linked to mutations in the MTHFR gene that upset the blood flow. Tests for the mutation are available.Research has found high doses of vitamin B6 and B12 and folate can help prevent these migraines.
3.A third type of migraine is the menstrual migraine, it is experienced by about 20 per cent of migraine sufferers. Sufferers have variations in genes related to hormone receptors and hormones stabilisation is important.
Medicines for migraines
Prescription Medicines that prevent migraine
Topirimate, Lyrica, Botox, ergotamine, beta blockers, flunarizine, methysergide, pizotifen, sodium valproate, tricyclic antidepressants
Prescription Medicines to treat migraines
Sumatriptan, Rizatriptan, almotriptan, eletriptan, frovatriptan, noratriptan, zolmitriptan.

Alternative therapies for Migraines
*Combination of these vitamins 2mg of folic acid, 25mg of vitamin B6 and 400mg of vitamin B12.
*Cephaly a medical device that treats migraine pain with neurostimulation the manufacturer claims it changes the trigger threshold of migraine headaches. As the pain threshold becomes harder to reach, migraine headaches are less frequent, less painful, or become less frequent.
*Cognitive Behavioural therapy involves identifying migraine triggers, changing lifestyle to avoid some triggers but exposing yourself to other triggers in a controlled way to reduce their ability to provoke a migraine. Found to produce a 77 per cent reduction in migraines.
Breakthrough new treatments on the horizon
Monoclonal antibodies that target a calcitonin gene-related peptide (CGRP), a neurotransmitter that is released from one nerve cell and activates the next one in a nerve tract during a migraine attack



